Problem solving and behavior modification
- PMID: 4938262
- DOI: 10.1037/h0031360

Publication types
- Affective Symptoms
- Behavior Therapy*
- Concept Formation
- Decision Making
- Information Theory
- Mental Disorders / therapy
- Orientation
- Personality
- Problem Solving*
- Programmed Instructions as Topic
- Psychological Theory
- Psychology, Clinical
- Set, Psychology
- Search Menu
- Sign in through your institution
- Advance Articles
- Author Guidelines
- Submission Site
- Open Access
- Self Archiving Policies
- Why publish with this journal?
- Call for Papers: Three Continuing Special Series
- About Annals of Behavioral Medicine
- About Society of Behavioral Medicine
- Editorial Board
- Advertising & Corporate Services
- Journals Career Network
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Acknowledgments, compliance with ethical standards.
- < Previous
Behavior Change Techniques and Their Mechanisms of Action: A Synthesis of Links Described in Published Intervention Literature
- Article contents
- Figures & tables
- Supplementary Data
Rachel N Carey, Lauren E Connell, Marie Johnston, Alexander J Rothman, Marijn de Bruin, Michael P Kelly, Susan Michie, Behavior Change Techniques and Their Mechanisms of Action: A Synthesis of Links Described in Published Intervention Literature, Annals of Behavioral Medicine , Volume 53, Issue 8, August 2019, Pages 693–707, https://doi.org/10.1093/abm/kay078
- Permissions Icon Permissions
Despite advances in behavioral science, there is no widely shared understanding of the “mechanisms of action” (MoAs) through which individual behavior change techniques (BCTs) have their effects. Cumulative progress in the development, evaluation, and synthesis of behavioral interventions could be improved by identifying the MoAs through which BCTs are believed to bring about change.
This study aimed to identify the links between BCTs and MoAs described by authors of a corpus of published literature.
Hypothesized links between BCTs and MoAs were extracted by two coders from 277 behavior change intervention articles. Binomial tests were conducted to provide an indication of the relative frequency of each link.
Of 77 BCTs coded, 70 were linked to at least one MoA. Of 26 MoAs, all but one were linked to at least one BCT. We identified 2,636 BCT–MoA links in total (mean number of links per article = 9.56, SD = 13.80). The most frequently linked MoAs were “Beliefs about Capabilities” and “Intention.” Binomial test results identified up to five MoAs linked to each of the BCTs ( M = 1.71, range: 1–5) and up to eight BCTs for each of the MoAs ( M = 3.63, range: 1–8).
The BCT–MoA links described by intervention authors and identified in this extensive review present intervention developers and reviewers with a first level of systematically collated evidence. These findings provide a resource for the development of theory-based interventions, and for theoretical understanding of intervention evaluations. The extent to which these links are empirically supported requires systematic investigation.
Behavior plays a key role in maintaining health, and in the prevention, management, and treatment of disease and disability. Activities such as smoking, alcohol misuse, physical inactivity, and certain dietary behaviors contribute to the global disease burden and often lead to premature death [ 1 , 2 ]. There has been a steady global increase in diseases attributed to behavioral risk factors, with substantial associated losses in national income. The need for effective and cost-effective health-related behavior change interventions is acute.
Despite rapid growth in behavioral intervention research, the effects of behavioral interventions continue to be typically small, variable, and not maintained long-term [ 3 , 4 ]. Cumulative progress in the design of more effective interventions could be improved by developing a more widely shared understanding of the “mechanisms of action” (MoAs) through which interventions bring about change [ 5 ]. A more thorough understanding of how and why interventions achieve their effects, through identification of the links between behavior change techniques (BCTs) and the MoAs they target, would enable us to (i) design interventions that include components more likely to be effective [ 6 ] and (ii) better explain intervention effects.
Behavioral interventions are often delivered as part of complex systems that include a number of BCTs. A BCT is defined as a replicable component of an intervention designed to alter or redirect causal processes that regulate behavior (i.e., a technique is proposed to be a potentially “active ingredient”). BCTs are designed to enable behavior change, and can do this by augmenting factors that facilitate behavior change, or by mitigating factors that inhibit behavior change. As an example, one might hypothesize that the BCT “Graded Tasks” (defined as: “set easy-to-perform tasks, making them increasingly difficult, but achievable, until behavior is performed” [ 7 ]) might change behavior by increasing beliefs about one’s capabilities. On the other hand, one might hypothesize that the BCT “Restructuring the Social Environment” (defined as: “change, or advise to change, the social environment in order to facilitate performance of the wanted behavior or create barriers to the unwanted behavior” [ 7 ]) might change behavior by decreasing negative social influences.
BCTs are usually selected on the basis of the theoretical constructs they are proposed to target; for example, prompting experience of mastery through behavioral practice is often used to increase self-efficacy, based on Bandura’s theory of self-efficacy [ 8 ]. However, links between the full range of BCTs that exist and the theoretical constructs they are believed to modify are not clearly understood, and the rationale underlying BCT selection is not always transparent in intervention articles.
To enhance the design of more effective interventions, we need to develop a clearer understanding of the processes through which individual BCTs have their effects (i.e., their MoAs) [ 9 ]. We conceptualize these MoAs as a range of theoretical constructs that represent the processes through which a BCT affects behavior. In this context, MoAs are constructs specified in theories of behavior and behavior change that can be seen to “mediate” intervention effects, such as “beliefs about capabilities,” “knowledge,” and “behavioral regulation.” They can be characteristics of the individual (i.e., intrapersonal psychological processes) and characteristics of the social and physical environment (e.g., social support).
Understanding the links between BCTs and MoAs is important not just for intervention development (i.e., for the purpose of selecting appropriate BCTs), but also for evaluation (i.e., for understanding the processes through which BCTs have their effects). Intervention evaluations, replications, and syntheses have benefitted, in recent years, from the development of guidance for reporting interventions, such as the Template for Intervention Description and Replication (TIDieR) [ 10 ], and BCT Taxonomy version 1 (BCTTv1) [ 7 , 11 ]. BCTTv1 is a classification system for characterizing the potentially active ingredients of behavioral interventions. It has been used to specify intervention techniques across a wide range of behavioral domains, for example physical activity [ 12 ], alcohol use [ 13 ], medication adherence [ 14 ], condom use [ 11 ], and behavior of health professionals [ 15 ]. It has also been applied in evidence syntheses to retrospectively identify BCTs used in published interventions and to evaluate their efficacy [ 16–19 ].
Such frameworks and taxonomies are helpful methods for knowledge accumulation and evidence synthesis; however, despite these advances, we currently lack a thorough understanding of the links between BCTs and specific MoAs. To advance understanding of these links, one approach is to review the published intervention literature and identify the links that have been identified by their authors. Previous research has suggested that empirical evidence about the links between individual BCTs and their MoAs may be limited [ 20 ]. However, by examining links that are explicitly described or hypothesized by authors within published articles of behavior change interventions [ 21 ], we can provide a first level of systematically collated evidence to shed light on the rationale researchers provide underlying their BCT selection, and help to elucidate the assumptions made by researchers about how intervention strategies have their effects.
This article reports on the first study from a larger program of research [ 9 ], examining links between BCTs and their MoAs. The current study aimed to identify the frequency with which specific BCTs are described as linked to specific MoAs. We drew on the published intervention literature to draw out the often-implicit assumptions made by researchers about (i) how to target theoretical constructs of interest (i.e., which BCTs target specific MoAs) and (ii) how interventions work (i.e., through which MoAs specific BCTs influence behavior). We also sought to understand whether or not any BCT–MoA links appeared with a relatively high level of frequency across the intervention literature.
How frequently is each possible BCT–MoA link described?
Which BCTs are frequently described as targeting a specific MoA?
Which MoAs are frequently described as influenced by a specific BCT?
Do any specific BCT–MoA links occur more frequently than might be expected given the average frequency of BCT–MoA links?
We identified published articles reporting behavior change interventions (both development and evaluation) in which authors described links between BCT(s) and MoA(s) (although they were not necessarily explicitly labeled as a “behavior change technique” or “mechanism of action” by the authors). To maximize efficiency, given time and resource constraints, our search strategy prioritized articles in which (i) BCTs had been identified using a taxonomy (BCTTv1, or one of the previous cross-behavior, or behavior-specific, taxonomies described in the introduction), either in the article itself (by intervention authors), or retrospectively by systematic reviewers, and/or (ii) MoAs had been identified using a theoretical framework. We identified articles through electronic searches, requests to experts, and by reviewing the reference lists of systematic reviews.
Electronic searches
To identify articles in which BCTs were likely to have been explicitly identified (to maximize efficiency of data extraction), we conducted a forward-search (i.e., a search of citations of a given paper) of five published BCT taxonomies [ 7 , 22–25 ]. To identify articles in which MoAs were likely to have been explicitly specified, we conducted a forward-search of the Theory Coding Scheme [ 26 ] and Theoretical Domains Framework [ 27 , 28 ]. All forward-searches were conducted within two online databases: Web of Science and Google Scholar.
Requests to experts
We sent a request for relevant articles to the 42 members of the project’s International Advisory Board ( http://www.ucl.ac.uk/behaviour-change-techniques/people/iab ), spanning 10 countries, and to researchers in the field via scientific and professional societies, including the US Society for Behavioral Medicine (SBM), European Health Psychology Society (EHPS), UK Society for Behavioural Medicine, and Division of Health Psychology of the British Psychological Society.
Reference lists of systematic reviews
The reference lists of all systematic reviews identified through the search methods above, including a review published by NICE as part of its behavior change guidance [ 29 ], were reviewed. Relevant articles were downloaded and screened for inclusion. By including intervention articles in which BCTs and/or MoAs had been coded retrospectively (i.e., through systematic review coding), we were not restricted to intervention articles that used the language of our set of BCTs and/or MoAs (e.g., articles in which a BCT was described using different labels to those used in the BCT Taxonomy). This also meant that we were not restricted to intervention articles that were dated after the publication of the various framework papers above.
Inclusion criteria
Intervention articles were included if they provided the description or evaluation of a behavior change intervention, and if the author(s) explicitly described a BCT (not necessarily labeled as such by the authors) as linked to one or more MoA(s) (i.e., there had to be at least one explicit, identifiable link between a BCT and an MoA). For example, an article would be included if the authors described an intervention that asked participants to set goals related to the target behavior, and indicated that goal-setting would change behavior through increasing self-regulation. Articles were excluded if they were not peer-reviewed (e.g., unpublished doctoral theses), if no behavioral outcome was reported, and/or if descriptions were not sufficiently detailed to be able to identify at least one link. For example, an article would be excluded if the authors described the intervention in detail, including BCTs, but did not explicitly state how any of the BCTs were expected to change the target behavior. Articles were also excluded where multiple BCTs were linked to multiple MoAs, but the specific links described were unclear. For example, an article would be excluded if it contained a table with a list of BCTs and a list of MoAs, where it was not possible to tell whether or not the authors were proposing that all of the BCTs were linked to all of the MoAs. No restrictions were made for year of publication, target behavior, journal, study quality, or article type.
Data Extraction
Two researchers initially reviewed the full texts of all identified articles for eligibility, with screening guidelines iteratively updated and all discrepancies resolved through discussion. Once acceptable inter-rater reliability was achieved (Kappa = 0.9), articles were screened independently (see Supplementary File 1 for a summary of inter-rater reliability across all stages of screening and coding).
BCTs were extracted from the included intervention articles using BCTTv1 [ 7 , 11 ] according to guidelines adapted from those on the BCTTv1 online training website ( www.bct-taxonomy.com ; see Supplementary File 2 for BCT coding guidelines). Examples of guidelines for BCT coding included: that BCTs should only be coded if they targeted one or more of the target behaviors or key preparatory behaviors of the intervention, that the whole intervention description should be read before beginning to code BCTs, and that, where BCTs were previously coded in the intervention articles using BCTTv1, the authors’ original coding was maintained; where an earlier taxonomy had been used [ 22 ], coding was updated in line with BCTTv1 guidelines. Two researchers who were trained in BCT coding independently coded BCTs (regardless of whether or not they were linked to an MoA) until inter-rater reliability was acceptable (Prevalence and Bias Adjusted Kappa [PABAK] = 0.9; see Supplementary File 1 ), at which point articles were coded initially by one researcher, and subsequently checked by one of two other researchers. Inter-rater reliability for BCT coding was assessed using PABAK [ 30 ], which accounts for high prevalence of negative agreement [ 11 ].
Coding links between BCTs and MoAs
Following BCT coding, links between BCTs and MoAs were extracted from the articles by two researchers independently. Coding these links was an iterative process, where discrepancies were resolved through discussion and coding guidelines revised accordingly (see Supplementary File 2 ). As we did not use a “finite” number of MoAs in data extraction, we used percentage agreement, rather than Kappa, to calculate reliability between coders.
A theoretical construct was extracted as an MoA provided it was (i) defined as a process through which behavior change could occur and (ii) clearly linked to a BCT. Discrepancies were resolved through discussion, and consulting with senior experts (S.M., M.J., A.J.R., M.d.B., M.P.K.) where needed. Guidelines for BCT–MoA link coding were revised when judged necessary to improve clarity (see Supplementary File 2 for final set of coding guidelines). Examples of BCT–MoA link coding guidelines included: that each BCT–MoA link should only be extracted once in any intervention description and that the most specific links possible should be coded (e.g., if BCT X was linked to “reinforcing factors” as an MoA, and reinforcing factors was said to include “feedback mechanisms and peer support,” BCT X was linked to feedback mechanisms and peer support, rather than “reinforcing factors”). To guide our coding, we drew on a set of 26 general MoAs; these were the 14 domains from the Theoretical Domains Framework [ 27 ] and the 12 additional most frequent MoA constructs from a set of 83 theories of behavior change [ 31 ] (see Appendix F of Supplementary File 2 for a full list of these 26 MoAs).
Data Synthesis
Extracted data were tabulated as follows. General information about the study (e.g., author, year, article and study type, target behavior, whether the authors identified a theoretical model as underpinning the development of the intervention) was entered into a “source” table; all identified BCTs were recorded in a “BCT” table; BCT–MoA link data were extracted into a “link” table. In the link table, each BCT–MoA link was assigned a unique row, to which the following information was added by two coders: BCT identity number (from BCTTv1 taxonomy), MoA label and definition (as described by the intervention authors), explicitness of the link (1 = some inference needed and 2 = no inference needed ), whether or not the links included groups of BCTs or MoAs (1 = one BCT linked to one MoA and 2 = more than one BCT linked to one MoA or more than one MoA linked to one BCT ), and whether the link was tested empirically (1 = MoA not measured and BCT–MoA link not tested , 2 = MoA measured but BCT–MoA link not tested , and 3 = BCT–MoA link tested ). The three tables were connected using an identifying code to ensure all data were available for each article.
Following data extraction, authors’ definitions of MoAs were categorized into the set of 26 general MoAs described earlier (i.e., 14 domains from the TDF [ 27 ] and 12 frequent MoA constructs from 83 theories of behavior change [ 31 ]). Two coders categorized MoAs until inter-coder reliability was >90% (see Supplementary File 3 for guidelines). Discrepancies were resolved through discussion, and MoAs that could not be categorized into any of the 26 were categorized as “other.”
To address our first three research questions (i.e., how frequently each possible BCT–MoA link is described, which BCTs are frequently described as targeting a specific MoA, which MoAs are frequently described as influenced by a specific BCT), we conducted descriptive analyses (in MS Excel) to examine the frequency of links between BCTs and MoAs (i.e., the number of articles in which a particular link was described).
In addition, to examine the relative frequency of each BCT–MoA link (i.e., our fourth research question), a series of one-tailed exact binomial tests was conducted (using R statistical software [ 32 ]) on the links for which MoAs could be categorized, comparing the observed with the expected frequency of occurrence for each link. In the absence of an agreed expected frequency of BCT–MoA links that could be used for comparison (i.e., H 0 ), we computed an expected value to serve as an estimate of the frequency that might be observed if BCTs were randomly linked to MoAs. The expected value was computed as the probability that a particular BCT was coded (frequency with which the BCT was linked with any MoA / total number of links between all BCTs and MoAs) multiplied by the probability a particular MoA was coded (frequency with which the MoA was linked with any BCT / total number of links between all BCTs and MoAs).
The resulting p values represent an indication of the likelihood of a link, allowing us to examine how frequently a specific BCT (X) was linked to a specific MoA (Y), by comparing this frequency with how often BCT X was used in any intervention, and how often MoA Y was targeted in any intervention. Because of the method used to compute an expected value, the resulting comparisons serve to identify links that are high in frequency relative to other links examined in this set of studies. Thus, a particular link may emerge as relatively frequent despite being identified a small number of times, if the BCT and/or MoA was rarely identified across the interventions. For example, if BCT X was linked with MoA Y only twice, but it was the only time MoA Y was linked to any BCT, the likelihood of this link may be greater than would be expected by chance (and would therefore be high in relative frequency, with a low p value). Conversely, if BCT X was linked to MoA Y eight times, but BCT X and MoA Y were both frequently linked to a range of other MoAs/BCTs, the likelihood of this link may not be greater than would be expected by chance (and would therefore be lower in relative frequency, with a larger p value).
We used p < .05 as an arbitrary minimum criterion for a BCT–MoA link, although clearly more or less stringent criteria can be applied to the resulting data. We are not making statistical inferences about links that meet, or do not meet, this criterion; rather, we are presenting the data in this way as an indication of the relative frequency of each link. We used a one-tailed test as the aim was to identify agreed-upon links rather than their absence.
The full results of the analyses (i.e., not just those that did not reach this threshold) are represented in “heat maps” of the findings. Heat maps allow individual data values to be represented as colors within a matrix to aid in interpreting the findings, and were generated through R [ 32 ]. The cells within the heat map contain a numerical value (i.e., p values) and are colored or shaded to reflect the relative strength or “heat” of that value (in this case, the relative frequency of a particular link).
The heat map clusters rows (i.e., BCTs) and columns (i.e., MoAs) by similarity, such that BCTs linked to similar MoAs are clustered together, and MoAs linked to similar numbers of BCTs are clustered together. MoAs that could not be categorized into one of our 26 (e.g., where there was not enough information in the article or the definition was unique and did not map on to any of our 26 definitions) were not included in these binomial tests. Thus, although we have selected one criterion for what constitutes a “link,” all of the data are available such that others can select alternative criteria as needed.
Characteristics of Included Studies
Of 974 intervention articles retrieved, 697 (72%) were excluded based on full-text screening. The most common reasons for exclusion were that intervention articles specified constructs as MoAs, but there were no clear links to individual BCTs, or that intervention articles linked BCTs to theoretical constructs, but did not identify these constructs as MoAs or hypothesized mediators. Of the remaining articles, 277 described at least one link, with years of publication ranging from 1982 to 2016 and 49% published in or after 2010. More than 10 behaviors were targeted by the interventions, including physical activity (40%), dietary behaviors (18%), alcohol reduction (10%), and smoking (6%). A majority (78%) were articles reporting outcome evaluations (rather than development papers or protocols). Approximately 14% of the articles did not mention any theoretical basis for the intervention. Thirteen percent of the articles mentioned theory, but without specifying how theory was applied to intervention development or evaluation. The analyses and discussions that follow are based on the 277 included articles. A full summary of study characteristics can be found on Open Science Framework (OSF) at https://osf.io/7qjvn/ .
Characteristics of Extracted Links
A total of 2,636 BCT–MoA links were extracted from the 277 articles, of which 33% required some inference to code, and 0.9% had been empirically tested within the included study. There were approximately 10 links per study ( M = 9.56, SD = 13.80), of which 88% included a group of BCTs linked to one MoA, or a group of MoAs linked to one BCT; 12% included a single BCT and a single MoA. Seventy-seven BCTs (of the 93 in BCTTv1) were coded across the 277 articles, 70 of which were linked to at least one MoA. The BCTs that were most frequently linked to an MoA were “Instruction on How to Perform the Behavior” (182 times) and “Problem Solving” (177 times). The most frequently linked MoA was “Beliefs about Capabilities” (734 times), followed by “Intention” (318 times). One of the MoAs from our pre-existing set of 26 was not identified: “Norms” (defined as “the attitudes held and behaviors exhibited by other people within a social group”). A full list of the 2,636 BCT–MoA links is available at https://osf.io/7qjvn/ .
Do Any Specific BCT–MoA Links Occur More Frequently Than Might Be Expected Given the Average Frequency of BCT–MoA Links?
Binomial tests were conducted to examine the relative frequency of BCT–MoA links. There were 87 links that met the criterion of p < .05, including 51 of 93 (55%) BCTs and 24 of 26 (92%) MoAs.
Up to eight BCTs were identified for each of the MoAs ( M = 3.63, range: 1–8), and up to five MoAs were identified for each of the BCTs ( M = 1.71, range: 1–5). For example, the MoA “Social Learning/Imitation” was linked to one BCT: “Demonstration of Behavior,” whereas the MoA “Attitude Towards the Behavior” was linked to eight BCTs: “Information about Health Consequences,” “Salience of Consequences,” “Information about Social and Environmental Consequences,” “Information about Emotional Consequences,” “Pros and Cons,” “Material Incentive (Behavior),” “Framing/Reframing,” and “Incompatible Beliefs.” Similarly, for BCTs, “Information about Health Consequences” was linked to the MoAs: “Knowledge,” “Beliefs about Consequences,” “Intention,” “Attitude Towards the Behavior,” and “Perceived Susceptibility/Vulnerability.”
Of the 25 MoAs (from our set of 26) that were linked to a BCT at least once, only “Optimism”—derived from the Theoretical Domains Framework [ 27 ]—was not linked to any BCT at the p < .05 threshold. Several BCTs, on the other hand, were coded frequently but did not meet the p < .05 threshold for any MoA. For example, the BCT “Review Behavior Goals” was coded 36 times, and “Social Support (Emotional)” was coded 14 times, but the relative frequency with which these were linked to an MoA did not meet the p < .05 threshold.
A heat map visually representing the frequency of BCT–MoA links (with darker colors representing p values closer to zero) is shown in Fig. 1 . These data are also available online as part of an interactive online tool ( https://theoryandtechniquetool.humanbehaviourchange.org/ ; see Discussion section for more details).

Heat map representing the relative frequency of BCT–MoA links. Each cell contains a numerical value (i.e., p value) and is colored to reflect the relative “heat” of that value (in this case, the relative frequency of a particular link). Knowledge = an awareness of the existence of something; Skills = an ability or proficiency acquired through practice; Social/ Professional Role and Identity = a coherent set of behaviors and displayed personal qualities of an individual in a social or work setting; Beliefs about Capabilities = beliefs about one’s ability to successfully carry out a behavior; Optimism = confidence that things will happen for the best or that desired goals will be attained; Beliefs about Consequences = beliefs about the consequences of a behavior (i.e., perceptions about what will be achieved and/or lost by undertaking a behavior, as well as the probability that a behavior will lead to a specific outcome); Reinforcement = processes by which the frequency or probability of a response is increased through a dependent relationship or contingency with a stimulus or circumstance; Intention = a conscious decision to perform a behavior or a resolve to act in a certain way; Goals = mental representations of outcomes or end states that an individual wants to achieve; Memory, Attention and Decision Processes = ability to retain information, focus on aspects of the environment, and choose between two or more alternatives; Environmental Context and Resources = aspects of a person’s situation or environment that discourage or encourage the behavior; Social Influences = those interpersonal processes that can cause oneself to change one’s thoughts, feelings or behaviors; Emotion = a complex reaction pattern involving experiential, behavioral, and physiological elements; Behavioral Regulation = behavioral, cognitive, and/or emotional skills for managing or changing behavior; Norms = the attitudes held and behaviors exhibited by other people within a social group; Subjective Norms = one’s perceptions of what most other people within a social group believe and do; Attitude towards the behavior = the general evaluations of the behavior on a scale ranging from negative to positive; Motivation = processes relating to the impetus that gives purpose or direction to behavior and operates at a conscious or unconscious level; Self-Image = one’s conception and evaluation of oneself, including psychological and physical characteristics, qualities, and skills; Needs = deficit of something required for survival, well-being, or personal fulfillment; Values = moral, social, or aesthetic principles accepted by an individual or society as a guide to what is good, desirable, or important; Feedback Processes = processes through which current behavior is compared against a particular standard; Social Learning/Imitation = a process by which thoughts, feelings, and motivational states observed in others are internalized and replicated without the need for conscious awareness; Behavioral Cueing = processes by which behavior is triggered from either the external environment, the performance of another behavior, or from ideas appearing in consciousness; General Attitudes/Beliefs = evaluations of an object, person, group, issue, or concept on a scale ranging from negative to positive; Perceived Susceptibility/Vulnerability = perceptions of the likelihood that one is vulnerable to a threat. BCT behavior change technique; MoA mechanism of action.
Table 1 describes the 51 BCTs and the MoAs to which they were most frequently linked. Thus, this table provides a summary of the MoAs through which these 51 BCTs may affect behavior, according to the authors of this set of published interventions. In some cases, there is one clear MoA for a given BCT; for example, the BCTs Goal Setting (Behavior) and Action Planning—both frequently coded across interventions—were only linked to “Behavioral Regulation” ( p = .003 and p =.001, respectively). In other cases, there are BCTs with links to multiple MoAs, but with one seemingly “dominant” MoA; for example, while the BCT “Problem Solving” was frequently linked to three MoAs, the link to “Beliefs about Capabilities” ( p = .008; occurring 65 times) was substantially more frequent than the next highest two: “Environmental Context and Resources” ( p = .026; occurring 9 times) and “Skills” ( p = .038; occurring 18 times).
BCT–MoA links with relatively high frequency in 277 intervention articles: Organized by BCT and presented in order of (i) BCT frequency from this study and (ii) p values
Numbers in parentheses for each BCT are as per BCTTv1. BCT behavior change technique; MoA mechanism of action; BCTTv1 BCT Taxonomy version 1.
It is also clear, based on the data in Table 1 , that the links may reflect hypothesized causal pathways, rather than mutually exclusive targeted constructs; for example, the BCT “Information about Health Consequences” was linked to the MoAs “Knowledge” ( p < .001), “Beliefs about Consequences” ( p < .001), “Attitude Towards the Behavior” ( p < .001), “Perceived Susceptibility/Vulnerability” ( p < .001), and “Intention” ( p = .004).
Table 2 describes the 24 MoAs and the BCTs to which they were most frequently linked. This table therefore provides a summary of the BCTs that could potentially be used to target these 24 MoAs, according to the authors of this set of published interventions. Again, in some cases, there is one clear BCT for a given MoA; for example, the MoA “Perceived Susceptibility/Vulnerability” was only linked to “Information about Health Consequences” ( p < .001), and the MoA “Social Learning/Imitation” was only linked to “Demonstration of the Behavior” ( p = .044). In other cases, multiple (theoretically linked) BCTs were linked to a given MoA; for example, the MoA “Emotion” was linked to “Anticipated Regret” ( p = .002), and “Information about Emotional Consequences” ( p = .024).
BCT–MoA links with relatively high frequency in 277 intervention articles: Organized by MoA alphabetically and presented in order of p values.
Findings from this study represent the first dataset summarizing hypothesized links between BCTs and MoAs that were frequently described by authors of published interventions. We identified 2,636 BCT–MoA links between 70 BCTs and 25 MoAs. Of those, 87 links met the p < .05 criterion. Identifying these links provides an initial resource of theoretical and practical value indicating which links are believed to be present (i.e., BCT X is frequently linked with MoA Y) and which links appear to be absent (i.e., BCT X is frequently identified but never linked with MoA Y).
In some cases, there is one clear BCT for a given MoA and one clear MoA for a given BCT. In other cases, there are BCTs linked to more than one MoA and MoAs linked to more than one BCT. There are a number of possible explanations for this—for example, for some constructs, relevant BCTs have been explicitly described in the theoretical literature. Intervention strategies to target self-efficacy (a conceptually identical construct to “Beliefs about Capabilities,” as defined in this study), for instance, have been explicitly identified in Bandura’s theory of self-efficacy [ 8 ]; the definitions Bandura provides of mastery experience, vicarious experience, and verbal persuasion are similar to the BCTs “Behavioral Practice/Rehearsal,” “Demonstration of the Behavior,” and “Verbal Persuasion about Capability,” respectively, all of which were linked to “Beliefs about Capabilities” in this study. In our study, “Beliefs about Capabilities” was the most frequently identified MoA across all articles, which may reflect the relative clarity with which this construct has been linked to BCTs within behavioral theories.
There are also BCTs and MoAs for which no clear links emerged. For example, there were two MoAs from our set of 26 for which no links were identified at the p < .05 level: “Optimism” (confidence that things will happen for the best or that desired goals will be attained) and “Norms” (the attitudes held and behaviors exhibited by other people within a social group). One possible explanation for this is that there may be a lack of clarity or agreement in the behavioral science community regarding the BCTs that can be used to target these MoAs. This is particularly problematic given that the MoA “Norms” occurs frequently in behavioral theories (see [ 31 ]). An alternative explanation is that researchers do not see these MoAs as being “modifiable” by BCTs, but rather see them as representing aspects of the individual (e.g., dispositional optimism) or environment (e.g., cultural norms) that may be difficult or impossible to target in behavioral interventions.
This research has also highlighted BCT–MoA links that have been identified but are infrequently used. For example, the BCT “Problem Solving” was linked to the MoA “Behavioral Regulation” 13 times; this did not meet the p < .05 criterion.
The heat map, and Tables 1 and 2 , can be viewed as a summary of intervention researchers’ beliefs about BCT–MoA links, and can be used as a starting point for intervention designers and evaluators. These data can be drawn upon to identify BCTs that have the potential to target relevant MoAs (e.g., for the purpose of intervention development) and, conversely, to understand the MoAs that individual BCTs are designed to target (e.g., for the purpose of intervention evaluation and theory development). To identify the likely “optimal” BCT–MoA link(s) (e.g., for the purpose of planning an intervention), one can refer to Tables 1 and 2 , which list the links that met the p < .05 criterion.
For instance, a researcher interested in increasing perceived vulnerability/susceptibility (e.g., drawing on the Extended Parallel Process Model [ 33 ]) may consider, based on our findings, that an appropriate BCT might be to provide information about the health consequences of the depicted unsafe/unhealthy behavior. Although some of the frequently identified links are intuitive, there are others that may be less immediately obvious (e.g., the link between the BCT “Mental Rehearsal of Successful Performance” and the MoA “Values”). By drawing on these findings, researchers may identify creative ways in which to target MoAs of interest (e.g., by including less commonly used BCTs).
Our findings can also be used to develop a framework for designing and conducting empirical tests of the BCT–MoA links, to guide the development of an evidence base that can resolve ambivalence about links, and to explore the potential of BCTs and MoAs that appear to be currently underused. Thus, the BCT–MoA links database can be used both to identify links that have been frequently described in the literature, for which empirical tests are needed, as well as to identify links that appear to be understudied. More broadly, advancing the science of behavior change at a theoretical and methodological level, through this and similar initiatives (e.g., see www.scienceofbehaviourchange.org ), helps to provide the grounding on which researchers and practitioners can build innovative interventions (e.g., by combining BCTs, knowing where important gaps are, and providing a basis for new hypotheses).
There are a number of additional points to emerge from this research. Seventy-two percent of the articles identified through our search methods did not explicitly describe links between BCTs and MoAs. These findings are consistent with previous meta-analytic findings, which indicated that, although 50% of the interventions reviewed reported a theoretical basis, 90% did not report links between all BCTs and individual theoretical constructs [ 20 ]. A common thread among guidelines for intervention development and evaluation [ 29 , 34 ] is the need for a strong and rigorously applied theoretical basis to optimize effectiveness and enhance our understanding of intervention effects [ 35 ]. Although many interventions state that they draw on theory when developing interventions, when descriptions of the links between theoretical constructs and individual BCTs are lacking, it can be difficult to draw generalizable theoretical conclusions.
Our findings point to a more general issue relating to theory use that has hampered intervention research: that conceptualizations of what constitutes “theory-based” are highly variable. A large number of interventions that are reported to be based on theory in fact draw on implicit or partially applied theories [ 20 , 36 , 37 ]. It is often unclear whether and/or how theory has been used in the selection of BCTs, and in the targeting and measurement of theoretical constructs that are considered to be mediating variables in the change process. Simply describing an intervention as having been informed by theory does not mean it has been [ 5 ]. To maximize the potential usefulness of theory, it is crucial that intervention articles replace implicit assumptions about how interventions have their effects with explicit statements as to how and why theoretical principles guiding the design of the intervention were applied and tested [ 31 , 38–40 ].
Finally, the finding that a majority of BCTs and MoAs were not linked individually by authors, but instead as groups of BCTs or MoAs may indicate that authors considered that there were synergistic relationships among BCTs and/or among MoAs (e.g., BCTs A, B, and C and/or MoAs X, Y, and Z work together in the behavior change process). Alternatively, it could point to a lack of specificity in the selection of BCTs and the targeting of MoAs, and/or to a lack of detail in intervention reporting.
Limitations
A number of limitations of the current work should be noted. The studies in this review were purposively selected to maximize the likelihood of identifying BCT–MoA links. In our call for articles, we contacted international societies with broad reach in North America (SBM) and Europe (EHPS); however, there are international societies covering other parts of the world that may have elicited further international research articles. Our dataset of articles may not be representative of the wider behavioral intervention literature; for example, the intervention literature may be restricted in the theories represented, and/or in how they represent the theories. We would note, however, that we did not set out to conduct a systematic review or to identify a representative sample of intervention articles; our aim was to identify a corpus of literature in which BCT–MoA links were most likely to be identifiable.
It should also be noted that the links extracted from the 277 articles were based on authors’ descriptions, and very few had been tested empirically within the articles. This suggests a clear research agenda: for researchers in behavior change to systematically test the links that have been frequently described. To this end, an initiative is underway in the United States to advance efforts to identify, measure, and manipulate MoAs through the experimental medicine approach ( www.scienceofbehaviourchange.org ; see also [ 41 ]).
The results of this study provide no information about the links that did not appear in the included study articles. The absence of reported links may reflect several possibilities: authors’ beliefs that such links do not exist, not considering these links when designing their studies, finding them too difficult to operationalize, using theoretical constructs and ideas implicitly, defaulting to common-sense assumptions about how behavior change happens, or not including this detail when reporting.
Finally, there are other characteristics of the studies, and BCT–MoA links, that we did not extract and that may be of interest and relevance (e.g., type of behavior change, such as initiation or maintenance, hypothesized interactive effects among BCTs, etc.). By publishing our dataset online through OSF and through our interactive online tool (see below), we welcome further data extraction and/or additional analyses by researchers who are interested in examining these characteristics. The findings from this study are informing a subsequent study that is bringing together other characteristics such as BCT delivery, behavioral target, intervention setting, and target population (see www.humanbehaviourchange.org ).
Future Research Directions
This is one of three related studies examining the links between BCTs and (i) MoAs and (ii) behavioral theories [ 9 ]. Findings from the current study will be triangulated with those from an expert consensus study involving 105 behavior change experts [ 42 ]. The triangulation exercise will provide an additional body of evidence by comparing the results in this study with current thinking by experts in the field, which will address many of the limitations associated with literature-based evidence. Together, these two data sets will provide an integrated matrix that will draw together the links described in published articles with those agreed by experts in the field. This suite of studies forms a key part of a larger program of research building an “ontology” of behavior change interventions that will extend relationships to modes of delivery, exposure, types of behaviors, populations, settings, and intervention effects (see www.humanbehaviourchange.org ). This program of work aims to advance our methods for intervention design, evaluation, and synthesis, creating an up-to-date knowledge base that can be tailored to specific populations, settings, and target behaviors.
Data Sharing
The data sets resulting from this study are available via the website OSF ( https://osf.io/7qjvn/ ) to ensure they are maximally transparent and useful to the scientific community. Publishing the data on OSF will enable research groups to identify new research questions and share data. By publishing our full matrix of links with all relevant data, we encourage researchers to examine the full matrix of links when drawing on the findings.
The findings from this study have contributed to two online resources for the research community. First, the BCT coding completed as part of this work (i.e., for 277 articles) is available as part of an existing resource that collates interventions specified by BCTs (see www.bct-taxonomy.com/interventions ). This online resource is searchable by author, year, BCT, and target behavior, and also includes a facility for researchers to add articles that have identified BCTs using BCTTv1. Second, the “heat map” matrix is available as an interactive tool for researchers and intervention developers ( https://theoryandtechniquetool.humanbehaviourchange.org/ ). For each link, users are able to access current study data, upload other data and information about relevant research activities, and contribute suggestions for collaborative research efforts to populate the matrix with empirical evidence ( www.humanbehaviourchange.org ). The more that programs of research in this area can be co-ordinated, the more efficiently evidence about BCT–MoA links will accumulate.
We would like to express our gratitude to all those who sent us peer-reviewed behavior change intervention descriptions for this study, to Dr. Emma Beard and Dr. Dan Dediu for their statistical input, and to all the researchers, particularly Holly Walton and Hilary Groarke, who assisted in the coding of reports and preparation of figures. This research is funded by UK Medical Research Council grant number MR/L011115/1.
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards Authors Rachel N. Carey, Lauren E. Connell, Marie Johnston, Alexander J. Rothman, Marijn de Bruin, and Michael P. Kelly have no conflicts of interest. Susan Michie is director of the Centre for Behaviour Change, University College London, which has received funds from industry and government agencies.
Authors’ Contributions The original study concept was developed by investigators Susan Michie, Marie Johnston, Alexander J. Rothman, Marijn de Bruin and Michael P. Kelly. The design of the study was developed by the investigators and researchers Rachel N. Carey and Lauren E. Connell and the implementation of the study was led by Rachel N. Carey and Lauren E. Connell, in collaboration with the investigators. Lauren E. Connell led the data analysis. Rachel N. Carey drafted the initial manuscript. All authors provided critical revisions to the document, and approved the final version of the manuscript for submission.
Ethical Approval The research outlined in this protocol paper has been approved by the University College London Research Ethics Committee (ID 6056/001). All procedures performed in the studies were conducted in accordance with the ethical standards of this committee.
Informed Consent This study did not involve primary data from human participants.
Bauer UE , Briss PA , Goodman RA , Bowman BA . Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA . Lancet . 2014 ; 384 : 45 – 52 .
Google Scholar
Kontis V , Mathers CD , Rehm J , et al. Contribution of six risk factors to achieving the 25 × 25 non-communicable disease mortality reduction target: A modelling study . Lancet . 2014 ; 384 : 427 – 437 .
Marteau T , Hollands GJ , Kelly M . Changing population behavior and reducing health disparities: Exploring the potential of “choice architecture” interventions . In: Kaplan RM , Spittel M , David DH , eds. Emerging Behavioral and Social Science Perspectives on Population Health . Rockville, MD : Agency for Healthcare Research and Quality and Office of Behavioral and Social Sciences Research: AHRQ Publication No. 15-0002 , 2015 .
Google Preview
Kwasnicka D , Dombrowski SU , White M , Sniehotta F . Theoretical explanations for maintenance of behaviour change: A systematic review of behaviour theories . Health Psychol. Rev . 2016 ; 10 : 277 – 96 .
Moore GF , Evans RE . What theory, for whom and in which context? Reflections on the application of theory in the development and evaluation of complex population health interventions . SSM Popul Health . 2017 ; 3 : 132 – 135 .
Onken LS , Carroll KM , Shoham V , Cuthbert BN , Riddle M . Reenvisioning clinical science: Unifying the discipline to improve the public health . Clin Psychol Sci . 2014 ; 2 : 22 – 34 .
Michie S , Richardson M , Johnston M , et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions . Ann Behav Med . 2013 ; 46 : 81 – 95 .
Bandura A . Self-efficacy: Toward a unifying theory of behavioral change . Psychol Rev . 1977 ; 84 : 191 – 215 .
Michie S , Carey RN , Johnston M , et al. From theory-inspired to theory-based interventions: A protocol for developing and testing a methodology for linking behaviour change techniques to theoretical mechanisms of action . Ann Behav Med . 2016 : 8 : 501 – 512 .
Hoffmann T , Glasziou P , Boutron I , et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide . Br Med J . 2014 : 348 – g1687 .
Webster R , Michie S , Estcourt C , et al. Increasing condom use in heterosexual men: Development of a theory-based interactive digital intervention . Transl Behav Med . 2016 ; 6 : 418 – 427 .
Devi R , Powell J , Singh S . A web-based program improves physical activity outcomes in a primary care angina population: Randomized controlled trial . J Med Internet Res . 2014 ; 16 : e186 .
Newbury-Birch D , Coulton S , Bland M , et al. Alcohol screening and brief interventions for offenders in the probation setting (SIPS Trial): A pragmatic multicentre cluster randomized controlled trial . Alcohol Alcohol . 2014 ; 49 : 540 – 548 .
Bobrow K , Brennan T , Springer D , et al. Efficacy of a text messaging (SMS) based intervention for adults with hypertension: Protocol for the StAR (SMS Text-message Adherence suppoRt trial) randomised controlled trial . BMC Public Health . 2014 ; 14 : 28 .
Treweek S , Bonetti D , Maclennan G , et al. Paper-based and web-based intervention modeling experiments identified the same predictors of general practitioners’ antibiotic-prescribing behavior . J Clin Epidemiol . 2014 ; 67 : 296 – 304 .
Gardner B , Smith L , Lorencatto F , Hamer M , Biddle SJ . How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults . Health Psychol Rev . 2016 ; 10 : 89 – 112 .
Sinnott C , Mercer SW , Payne RA , Duerden M , Bradley CP , Byrne M . Improving medication management in multimorbidity: Development of the MultimorbiditY COllaborative Medication Review And DEcision Making (MY COMRADE) intervention using the Behaviour Change Wheel . Implement Sci . 2015 ; 10 : 132 .
Alkhaldi G , Hamilton FL , Lau R , Webster R , Michie S , Murray E . The effectiveness of prompts to promote engagement with digital interventions: A systematic review . J Med Internet Res . 2016 ; 18 : e6 .
Bull ER , Dombrowski SU , McCleary N , Johnston M . Are interventions for low-income groups effective in changing healthy eating, physical activity and smoking behaviours? A systematic review and meta-analysis . BMJ Open . 2014 ; 4 : e006046 .
Prestwich A , Sniehotta FF , Whittington C , Dombrowski SU , Rogers L , Michie S . Does theory influence the effectiveness of health behavior interventions? Meta-analysis . Health Psychol . 2014 ; 33 : 465 – 474 .
Peters GJ , de Bruin M , Crutzen R . Everything should be as simple as possible, but no simpler: Towards a protocol for accumulating evidence regarding the active content of health behaviour change interventions . Health Psychol Rev . 2015 ; 9 : 1 – 14 .
Abraham C , Michie S . A taxonomy of behavior change techniques used in interventions . Health Psychol . 2008 ; 27 : 379 – 387 .
Michie S , Hyder N , Walia A , West R . Development of a taxonomy of behaviour change techniques used in individual behavioural support for smoking cessation . Addict Behav . 2011 ; 36 : 315 – 319 .
Michie S , Whittington C , Hamoudi Z , Zarnani F , Tober G , West R . Identification of behaviour change techniques to reduce excessive alcohol consumption . Addiction . 2012 ; 107 : 1431 – 1440 .
Michie S , Ashford S , Sniehotta FF , Dombrowski SU , Bishop A , French DP . A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: The CALO-RE taxonomy . Psychol Health . 2011 ; 26 : 1479 – 1498 .
Michie S , Prestwich A . Are interventions theory-based? Development of a theory coding scheme . Health Psychol . 2010 ; 29 : 1 – 8 .
Cane J , O’Connor D , Michie S . Validation of the theoretical domains framework for use in behaviour change and implementation research . Implement Sci . 2012 ; 7 : 37 .
Michie S , Johnston M , Abraham C , Lawton R , Parker D , Walker A ; “Psychological Theory” Group . Making psychological theory useful for implementing evidence based practice: A consensus approach . Qual Saf Health Care . 2005 ; 14 : 26 – 33 .
National Institute for Health and Care Excellence (NICE) . Behaviour Change: Individual approaches . 2014 ; 49 . Available at http://guidance.nice.org.uk/ph49 .
Byrt T , Bishop J , Carlin JB . Bias, prevalence and kappa . J Clin Epidemiol . 1993 ; 46 : 423 – 429 .
Michie S , West R , Campbell R , Brown J , Gainforth H. ABC of Behaviour Change Theories . Sutton, Surrey, UK : Silverback Publishing ; 2014 .
R-Package . A language and environment for statistical computing . Vienna, Austria : R Foundation for Statistical Computing ; 2013 .
Witte K . Putting the fear back into fear appeals: The extended parallel process model . Communications Monographs . 1992 ; 59 : 329 – 349 .
Craig P , Dieppe P , Macintyre S , Michie S , Nazareth I , Petticrew M ; Medical Research Council Guidance . Developing and evaluating complex interventions: The new medical research council guidance . BMJ . 2008 ; 337 : a1655 .
Sniehotta FF , Presseau J , Araújo-Soares V . On the development, evaluation and evolution of health behaviour theory . Health Psychol Rev . 2015 ; 9 : 176 – 189 .
Arnott B , Rehackova L , Errington L , Sniehotta FF , Roberts J , Araujo-Soares V . Efficacy of behavioural interventions for transport behaviour change: Systematic review, meta-analysis and intervention coding . Int J Behav Nutr Phys Act . 2014 ; 11 : 133 .
Bernard P , Carayol M , Gourlan M , et al. Moderators of theory-based interventions to promote physical activity in 77 randomized controlled trials . Health Educ Behav . 2016 : 1090198116648667 .
Rothman AJ , Klein WM , Cameron LD . Advancing innovations in social/personality psychology and health: Opportunities and challenges . Health Psychol . 2013 ; 32 : 602 – 608 .
French SD , Green SE , O’Connor DA , et al. Developing theory-informed behaviour change interventions to implement evidence into practice: A systematic approach using the Theoretical Domains Framework . Implement Sci . 2012 ; 7 : 38 .
Prestwich A , Webb TL , Conner M . Using theory to develop and test interventions to promote changes in health behaviour: Evidence, issues, and recommendations . Curr Opin Psychol . 2015 : 5 : 1 – 5 .
Sheeran P , Klein WM , Rothman AJ . Health behavior change: Moving from observation to intervention . Annu Rev Psychol . 2017 ; 68 : 573 – 600 .
Connell LE , Carey RN , Johnston M , Rothman AJ , de Bruin M , Kelly MP , Michie S . Links between behaviour change techniques and mechanisms of action: an expert consensus study . 2018 . In press . doi:10.31234/osf.io/fge86
Supplementary data
Email alerts, citing articles via.
- X (formerly Twitter)
- Recommend to Your Librarian
- Advertising and Corporate Services
Affiliations
- Online ISSN 1532-4796
- Print ISSN 0883-6612
- Copyright © 2024 Society of Behavioural Medicine
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Family-Based Treatments for Disruptive Behavior Problems in Children and Adolescents: An Updated Review of Rigorous Studies (2014-April 2020)
Ashli j sheidow , ph.d., michael r mccart , ph.d., tess k drazdowski , ph.d..
- Author information
- Article notes
- Copyright and License information
Ashli J. Sheidow, Ph.D., is a Senior Research Scientist at OSLC in Eugene, Oregon.
Michael R. McCart, Ph.D., is a Senior Research Scientist at OSLC in Eugene, Oregon.
Tess K. Drazdowski, Ph.D., is a Research Scientist at OSLC in Eugene, Oregon.
Author Contact: Ashli J. Sheidow: OSLC, 10 Shelton McMurphey Blvd., Eugene, OR, 97401; [email protected] ;
Issue date 2022 Jan.
Disruptive behavior problems in youth are common and costly, lead to adverse outcomes, and are often left untreated. This paper builds on previous work by providing an updated evaluation of family-based treatments based on results from randomized controlled trials (RCTs) for three populations: (1) children with disruptive behavior, (2) adolescents with disruptive behavior, and (3) adolescents with juvenile justice involvement. Using a comprehensive process, 28 new reports on 27 RCTs were identified for the 2014-April 2020 period, which when combined with the prior evidence base of all rigorous RCTs, resulted in 3 well-established , 11 probably efficacious , and 7 possibly efficacious family-based treatment categories. Many of the RCTs lent further support to existing treatment categories, more countries were represented, and several RCTs incorporated technology. Notable issues that remain include a limited number of family-based treatments for adolescents and for youth with juvenile justice involvement, as well as methodological concerns.
Keywords: disruptive behavior, delinquency, family therapy, parenting, evidence-based practice
Introduction and State of Evidence
Overview of the condition.
This article reviews the empirical literature to date on family-based treatments for children and adolescents with disruptive behavior (DB) problems. Such behavior is prevalent and costly, and it is a common reason for referrals to mental health treatment and/or the juvenile justice (JJ) system. U.S. data from the National Survey of Children’s Health revealed that 7.4% of youth aged 3 to 17 years had a current behavioral or conduct problem, and 47% of those youth did not receive treatment ( Ghandour et al., 2019 ). Globally, 1.5% of female youth and 3.7% of male youth have conduct disorder, accounting for 5.75 million years of healthy life lost ( Erskine et al., 2014 ). Of note, these figures only capture youth with significant clinical presentations of DB and not those with significant DB who are undiagnosed. Youth with DB are also placed in the JJ system, which processes 1 million new cases a year in the U.S. ( Hockenberry & Puzzanchera, 2018 ). Youth with DB are at risk for a variety of adverse long-term outcomes, including school dropout, compromised mental health (e.g., depression, anxiety, substance use, suicidal behaviors), family and relationship problems, and economic problems up to 40 years later ( Colman et al., 2009 ). Effective treatment can help reduce these risks and associated costs.
The present review focuses on treatments for serious DB (e.g., aggression, rule-breaking, property destruction, stealing) often resulting in a diagnosis of oppositional defiant disorder (ODD) or conduct disorder (CD), as defined in the Diagnostic and Statistical Manual of Mental Disorders , and/or involvement with the JJ system. Youth involved in the JJ system tend to exhibit more severe behaviors and needs compared to typical disruptive youth; since treatments for these youth need to address these complex concerns, the present review examined the evidence for this population separately.
Summary of Prior Evidence Base
The prior Journal of Marital and Family Therapy (JMFT) review on family-based treatments for youth with DB broadly ( Henggeler & Sheidow, 2012 ) was limited to treatments (a) for adolescents, (b) with multiple randomized controlled trials (RCTs), (c) with at least one RCT conducted by a team independent of the developer(s), and (d) with effects sustained at least one year. While it was typical for reviews at that time to focus on the highest level of the evidence base ( “empirically supported treatments” ), these criteria severely limited the applicable empirical literature reviewed. Further, the focus was adolescents, so the previous JMFT review excluded treatments for children altogether. Other prior JMFT reviews addressed some of these shortcomings. For example, Kaslow and colleagues (2012) reviewed family-based treatments for a range of disorders, including treatments for ODD in children, and reviewed evidence from RCTs as well as “promising interventions” that had yet to have RCT data. Baldwin and colleagues (2012) completed a meta-analysis of RCTs of specific family therapies for adolescent delinquency, CD, and substance use (i.e., Brief Strategic Family Therapy [BSFT], Functional Family Therapy [FFT], Multidimensional Family Therapy [MDFT], Multisystemic Therapy [MST]) adding statistical evidence to the effectiveness of these adolescent treatments.
Subsequent to these reviews, more detailed evaluation criteria for psychosocial treatments were specified ( Southam-Gerow & Prinstein, 2014 ). Since then, reviews tend to rely on this multi-level specification, identifying treatments as well-established , probably efficacious , possibly efficacious, experimental, or of questionable efficacy (Levels are detailed in Method section). Importantly, Southam-Gerow and Prinstein also defined rigor in treatment studies, including RCT design, measurement, and reproducibility criteria. In recent years, there have been two comprehensive reviews relevant to DB, both of which used the Southam-Gerow and Prinstein instructions. The first reviewed all psychosocial treatment studies for adolescent DB through December 2014 ( McCart & Sheidow, 2016 ); the second reviewed all psychosocial treatment studies for childhood DB through October 2016 ( Kaminski & Claussen, 2017 ). These built upon a prior review by Eyberg et al. (2008) and collectively categorized the entire prior empirical literature (i.e., 48 years of psychosocial treatment research) using the Southam-Gerow and Prinstein levels. Overall, these previous reviews and meta-analyses have found support for behavioral therapy treatment types for DB in children and combinations of behavior therapy, cognitive-behavior therapy (CBT), and family therapy for adolescents while acknowledging limitations such as focusing on limited populations or treatment models.
Current Study
The current study (1) reviewed family-based treatments for DB published since prior reviews (i.e., 2014 to April 2020) and (2) updated the evidence base classifications for three areas (children with disruptive behavior, adolescents with disruptive behavior, adolescents with juvenile justice involvement) using all available literature to date (through April 2020). This expands significantly on prior reviews by including the entirety of previous rigorous evidence for both childhood and adolescence in one review and including all treatments with at least one rigorous RCT, casting a broader net for potential inclusion of evidence-based treatments. Due to space limitations and the enormous literature of non-RCT DB studies, this update was limited to studies meeting the five methods criteria for rigor ( Southam-Gerow & Prinstein, 2014 ).
This update used a two-stage, multi-step process to identify and code relevant articles, and to integrate the newly identified RCTs with the prior evidence base of rigorous RCTs on family therapy for DB (i.e., Kaminski & Claussen, 2017 ; McCart & Sheidow, 2016 ).
Stage I: Empirical Literature Since Prior Reviews
Step one: record identification..
A wide range of terms were searched in PsycINFO and PubMed: disruptive behavior, aggression, behavior problems, conduct disorder, oppositional defiant disorder, child behavior disorders, offending, or delinquency, each cross-referenced with therapy, treatment, or intervention . Searches were limited to peer-reviewed, English-language articles published from January 2014 to April 2020 and focused on youth. Duplicates were removed, for a total 16,819 records (see Figure 1 PRISMA diagram).
Figure 1. PRISMA Flow Diagram of Search and Selection Process for Stage 1: Empirical Literature Since Prior Reviews [2014-April 2020].
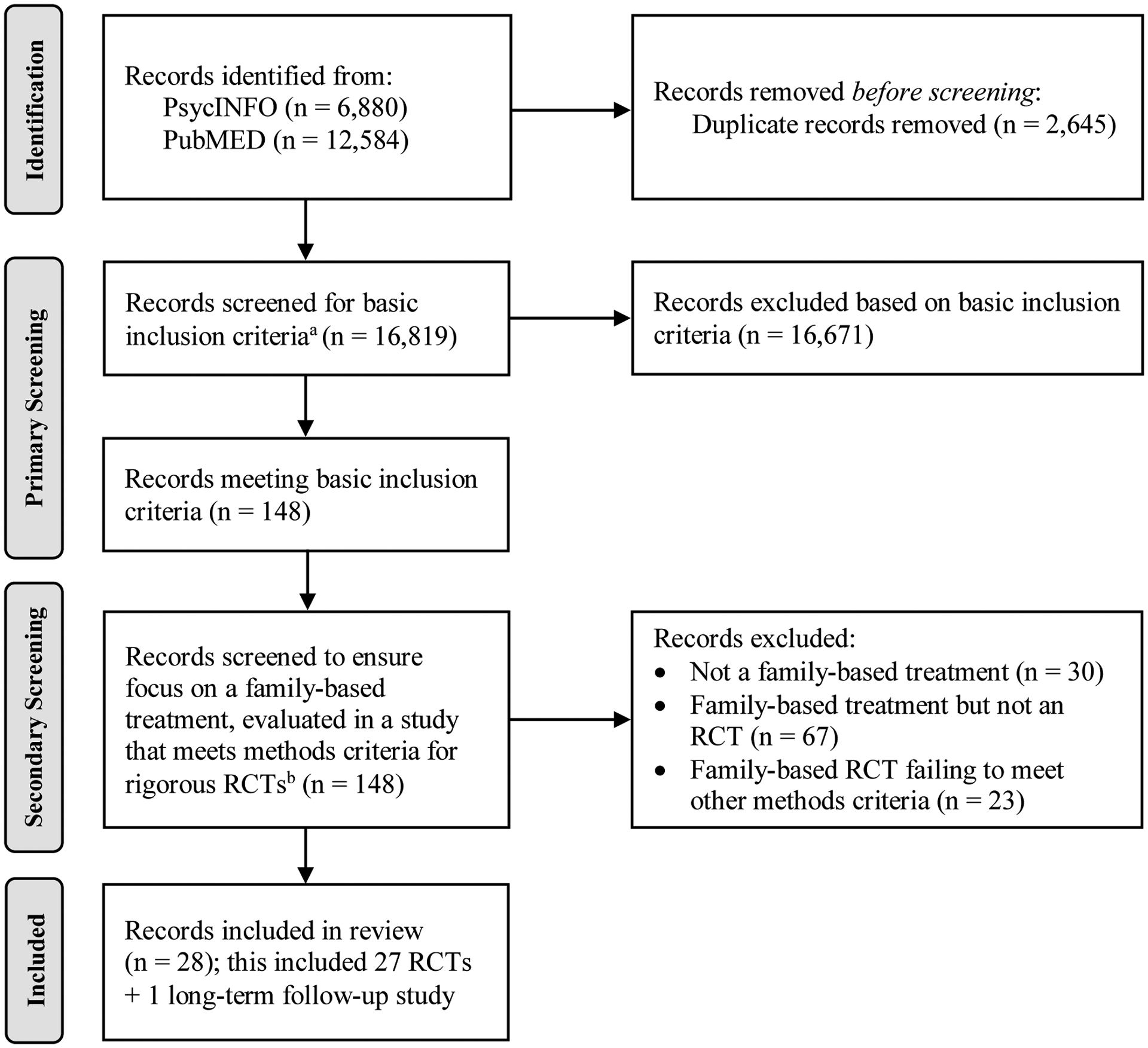
Note. RCT = randomized controlled trial.
a Basic inclusion criteria are as follows: (1) focus on youth aged 3–19; (2) focus on disruptive behavior as a primary problem; and (3) evaluation of a psychosocial treatment that could be delivered in a community-based setting. Treatments requiring a (1) school-wide or classroom-based intervention, (2) facility outside the youth’s typical community (e.g., inpatient facility, wilderness camp), or (3) system-wide change in the way an existing facility operates (e.g., program requiring the entire JJ system to change operations) were excluded.
b Regarding methods criteria, studies had to (1) involve an RCT design; (2) have treatments with manuals or a logical equivalent; (3) be conducted with a population treated for specified problems, for whom inclusion criteria were clearly delineated in a reliable, valid manner; (4) use reliable and valid outcome assessment measures gauging disruptive behavior problems; and (5) use appropriate data analyses and a sample size sufficient to detect expected effects (generally accepted as at least one condition with at least 20 cases and intent-to-treat research methods).

Step two: primary screening.
Trained assistants reviewed abstracts to identify studies meeting basic inclusion criteria. First, articles needed to focus on youth aged 3 to 19. If age extended above or below this, the study was included if M age = 3–19. Second, youth needed to have DB at baseline (e.g., diagnosis, clinical level scores, selection due to behaviors such as a JJ sample) and studies needed to target DB as a primary problem. Studies in which the behaviors were solely due to attention-deficit hyperactivity disorder, substance use, sexual offending, or autism or where these were the focus of treatment were excluded because separate and extensive bodies of literature focus on such treatments. Third, studies needed to evaluate psychosocial treatments with therapeutic intent that could be delivered in community-based settings. Treatments requiring a (1) school-wide or classroom-based intervention, (2) facility outside the youth’s typical community (e.g., inpatient facility, wilderness camp), or (3) system-wide change (e.g., requiring the entire JJ system to change operations) were excluded. However, stand-alone treatments studied within one of these milieus that could logically be delivered in a community setting (e.g., CBT delivered while youth were detained) were considered, as were programs that could feasibly be implemented in a community without requiring system-wide change (e.g., converting a subset to be specialized treatment foster care homes vs. requiring all foster homes to change practices). If there was insufficient information in an abstract, the full text was reviewed to confirm criteria. Records ( n = 148) meeting these basic criteria were promoted to step three.
Step three: secondary screening.
The first and second authors reviewed full texts of all promoted records to ensure the focus was on a family-based treatment. To be inclusive, criteria were any treatments in which parents were included in the individuals being intervened upon (e.g., parenting skills, parent-youth communication training, parent-youth relationship). This step also determined if the study met criteria for rigorous RCTs ( Southam-Gerow & Prinstein, 2014 ), with a focus on being as inclusive as possible: (1) RCT design; (2) a treatment manual or logical equivalent (e.g., detailed treatment descriptions that could provide for replicability); (3) a DB population for whom inclusion criteria were clearly delineated in a reliable, valid manner (e.g., diagnosis, clinical level scores, JJ sample); (4) reliable and valid outcome assessment measures gauging DB problems (e.g., clinical assessment, re-arrests); (5) appropriate data analyses and a sample size sufficient to detect expected effects (generally accepted as intent-to-treat research methods and at least one condition with at least 20 cases or via the RCT authors’ power analyses). Records promoted were 27 RCTs, plus 1 long-term follow-up study.
Step four: study coding.
The first and second authors coded the promoted family-based, rigorous RCTs and extracted data regarding participant demographics; treatment name; treatment type (determined based on the approach used to elicit behavior change: Behavior Therapy protocols elicited change via behavior modification techniques, CBT relied primarily on cognitive strategies to elicit behavior change, Family Therapy elicited change by targeting the family system and relationships, and some treatments used multiple approaches and were labeled as such); delivery method (e.g., Family Groups, Parent Groups ); treatment setting (e.g., Home, Clinic ); country; therapist (e.g., Student, Master’s-level ); informants for DB measures ( Observation, Official records, Parent, Self, or Teacher ); and length of assessment post-baseline. For each statistical test conducted with a DB outcome (e.g., analysis of change over time, test of a group difference at posttreatment), the treatment was evaluated as superior to , equivalent to , or inferior to the comparison condition. Consistent with previous reviews, a study was considered Supportive of the target treatment if the treatment was (a) superior to an active placebo or treatment, (b) superior to a waitlist or no-treatment comparison, or (c) equivalent to an already well-established treatment on at least 50% of the DB outcome measures.
Stage II: Integration of Stage I Results with the Prior Evidence Base
Step one: rcts identified in prior reviews..
Methods for the present review were structured such that the search criteria and processes were consistent with the prior reviews that used the Southam-Gerow and Prinstein (2014) classifications. Those prior reviews listed all rigorous RCTs for children ( Kaminski & Claussen, 2017 ) and adolescents ( McCart & Sheidow, 2016 ), and both are publicly available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5600477/ ; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5055452/ . From these lists, all family-based RCTs were identified by reading each publication that potentially included parents or a family focus, and using the same selection criteria as used in the present review (see above). The same coding method described above for treatment type and delivery method was applied to these RCTs to assist with identifying treatment categories rather than focusing only on specific “named” treatments (see Southam-Gerow & Prinstein instructions). Each RCT was designated as Superior to Waitlist/No Treatment, Superior to Active Placebo/Treatment, or Equivalent to Already Well-Established Treatment on at least 50% of the DB outcomes.
Studies indicate that the types of DB exhibited by youth vary significantly with age (e.g., Lahey et al., 2000 ), and the proximal causes and correlates of DB vary across earlier and later stages of child development (e.g., Fleming et al., 2010 ). Therefore, effective treatments for children and adolescents must focus on a slightly different array of targets. Similarly, given the personal, familial, and societal consequences, JJ behaviors command a differing treatment intensity compared to a lower level of DB. Thus, treatments were categorized as being for children ( M age in the RCT below 12) or for adolescents ( M age of 12–19), and treatments for JJ-involved youth were identified consistent with McCart and Sheidow (2016) .
Step two: level of support classifications.
Classifications were made following the Southam-Gerow and Prinstein (2014) instructions, based on all published RCTs to date that were Supportive of the target treatment. Specifically, well-established (Level 1) treatments have at least two rigorous RCTs, conducted by at least two distinct research teams, demonstrating the target treatment is either 1.1a) significantly superior to an active placebo or treatment or 1.1b) equivalent to a well-established treatment. Probably efficacious (Level 2) treatments have 2.1) at least two rigorous RCTs showing the target treatment is significantly superior to waitlist or no-treatment group or 2.1) at least one rigorous RCT meeting 1.1a or 1.1b criteria. Possibly efficacious (Level 3) treatments have 3.1) at least one rigorous RCT with evidence of superior treatment effects compared to waitlist or no treatment. Of note, Southam-Gerow and Prinstein also allow treatments to be deemed possibly efficacious if 3.2) at least two non-randomized studies show the treatment is efficacious. However, that was not relevant for the current update since this review focused exclusively on rigorous RCTs. Similarly, experimental treatments (Level 4) were not included here as that category does not require RCTs. Finally, treatments of questionable efficacy (Level 5) include those tested in RCTs and found inferior (i.e., produced no beneficial effect) when compared to another treatment, waitlist, or no-treatment group.
Figure 1 summarizes the identification and inclusion of studies. As described in the Method section, most records were excluded during the Primary Screening; that is, they failed to meet one or more of the basic inclusion criteria (see Method section) such as focusing on an excluded sample (e.g., autism) and/or not evaluating a psychosocial treatment. In the Secondary Screening, records were excluded because they were not an RCT ( n = 67), did not focus on a family-based treatment ( n = 30), or failed to meet other methods criteria ( n = 23). This resulted in 28 records that reported on 27 rigorous RCTs (i.e., 1 article is a follow-up report).
Table 1 lists the coded data extracted. Overall, this update ( n of the 27 RCTs is listed in parentheses) found that the majority of the target treatments examined in RCTs since previous reviews were conducted in clinic (12) or university/hospital settings (2), but there was some expansion from primarily office-based treatments: some were home-based (4), delivered via phone and/or Internet (6), or school-based (2). One did not report setting. Similar trends were seen for providers of services. Most treatments were provided by professional therapists (20) or clinical students (1), but trials also expanded to services provided by an array of individuals: foster care workers and case managers (2), Bachelor’s-level coaches (1), and even caregiver self-directed models (2). One did not report provider. As observed in past research on DB, the majority (21) of new RCTs focused on children, with only 6 on youth over M age = 12. Similar to previous reviews, treatments utilizing Behavior Therapy with parents and families, on its own (19), with the addition of CBT (3), and with the addition of CBT and Family Therapy (2), continued to be the most widely tested and consequently have the strongest support (3 RCTs tested Family Therapy on its own). A wide range of delivery methods have been tested for treatment of DB since previous reviews: Family, Family Groups, Family via Internet, Parent Coaching, Parent Groups, Parent Individual, Parent Self-Directed, Child Groups, and/or Child Individual. Twelve RCTs included multi-component treatments that combined delivery methods (e.g., Child-only methods were always in tandem with other family-based methods). Continued testing of services in countries outside of the U.S. (6) was also observed: Australia (4), Belgium (1), Canada (1), China (1), Finland (1), Ireland (1), Israel (1), The Netherlands (3), New Zealand (1), Norway (1), Portugal (1), Sweden (2), and the U.K. (3). Further, 14 of the new RCTs were conducted by investigators independent from the treatment developers. In summary, of the 27 RCTs, 15 found support for the target treatment compared to a Waitlist/No Treatment (8), Active Placebo/Treatment (6), or Already Well-Established Treatment (1).
Rigorous Studies a for Disruptive Behavior [2014-April 2020] Identified Since Prior Reviews (by Treatment Type b )
- M.1 Group design: Study involved a randomized controlled design
- M.2 Independent variable defined: Treatment manuals or logical equivalent were used for the treatment
- M.3 Population clarified: Conducted with a population, treated for specified problems, for whom inclusion criteria have been clearly delineated in a reliable, valid manner
- M.4 Outcomes assessed: Reliable and valid outcome assessment measures gauging the problems targeted (at a minimum) were used
- M.5 Analysis adequacy: Appropriate data analyses were used and sample size was sufficient to detect expected effects
Type refers to Behavior Therapy; Behavior Therapy & Cognitive-Behavior Therapy; Behavior Therapy, Cognitive-Behavior Therapy, & Family Therapy; Family Therapy
Delivery Method refers to Family; Family Groups; Family via Internet; Parent Coaching; Parent Groups; Parent Individual; Parent Self-Directed; Child Groups; and/or Child Individual (Child-only options were always in tandem with other family-based methods)
Indicates studies that are by investigators independent from the treatment developers.
Samples denoted as JJ contain primarily juvenile justice-involved participants.
NR = Not Reported
Primary ethnicities are reported. AA = African American; C = Caucasian; H = Hispanic; Nat A = Native American.
TAU = Treatment as Usual
O = Observation; P = Parent- or caregiver-report; R = Official records; S = Self-report; T = Teacher-report.
This column indicates the number of disruptive behavior measures in the study that showed a statistically significant ( p < .05) between-group difference favoring the target treatment. For example, an entry of 2/3 would indicate that the study included 3 measures of disruptive behavior and that the experimental treatment showed significantly better outcomes than the control condition on 2 of the measures.
For the 2 studies where the condition sizes were not reported, the total sample size was available and was sufficiently large ( n = 1,805 and n = 205) in these two-condition studies such that mathematically one of the two conditions would have been n = 20+.
Studies Supportive of the target treatment in either the current review ( n = 16), Kaminski and Claussen (2017 ; n = 20), or McCart and Sheidow (2016 ; n = 20) were used to determine the Level of support based on the Criteria for Classifying Evidence-Based Psychosocial Treatments specified by Southam-Gerow and Prinstein (2014) . The Supplemental Table summarizes all 56 publications, including full citations, of rigorous RCTs by treatment category and population (i.e., Children with DB, Adolescents with DB, Adolescents with JJ-Involvement). Table 2 lists the treatment categories falling into Levels 1–3. No previously or newly identified family-based treatments were proven in an RCT to be inferior to another treatment, waitlist, or no-treatment group, so there were no treatments of questionable efficacy (Level 5). Of note, treatment categories were derived from a combination of treatment type (i.e., Behavior Therapy , Cognitive-Behavior Therapy [ CBT ], Family Therapy ) and delivery method. So, for example, Behavior Therapy for DB in children delivered within individual families is well-established (Level 1), but when delivered to multiple families meeting in groups, it is probably efficacious (Level 2).
Cumulative a Level of Support Designations for Disruptive Behavior Treatments
Note: JJ = juvenile justice.
Cumulative support is from randomized controlled trials included in prior reviews (Brestan & Eyberg, 1998; Eyberg et al., 2008 ; Kaminski & Claussen, 2017 ; McCart & Sheidow, 2016 ) and the current review.
Treatments listed as being for Children included studies in which the mean age fell below 12-years, while those listed as being for Adolescents included studies in which the mean age fell between 12 and 19 years.
Treatment is specifically designed for two-parent families.
Level 3 designation in the present review was limited to examining randomized controlled trials meeting the methods criteria defined by Southam-Gerow and Prinstein (2014) .
Well-Established (Level 1).
There are three well-established treatment categories, two for Children with DB and one for Adolescents with JJ-Involvement.
Children with DB.
Behavior Therapy delivered either via parent groups or via family sessions continues to be well-established . Using behavior modification principles, where desired behaviors are reinforced and undesired behaviors are ignored or given negative consequences (e.g., time out, privilege loss), Behavior Therapy with parents and families teaches parents effective child behavior management skills and improving the parent-child relationship through such practices as providing specific praise, creating house rules, and using charts and other incentive systems. Supplemental Table 1 provides a complete list, but some specific examples of these behavioral treatments include Incredible Years Basic, Standard Triple P, COMET/KOMET Groups, and Parent-Child Interaction Therapy (PCIT) delivered to individual families.
Adolescents with DB.
Currently, there are no well-established treatments.
Adolescents with JJ-Involvement.
Incorporating Behavior Therapy, CBT, and Family Therapy delivered via a combination of family, parent, and child sessions is well-established . Treatments in this category are MST and Treatment Foster Care Oregon (TFCO). These target DB by using many of the behavioral principles described above and offering 24/7 support to families through a treatment team approach. They also include individual and skill-building sessions with the youth and parents using CBT tenets by teaching different ways to change thinking patterns and improving problem-solving and coping skills. Often, while in treatment, multiple stakeholders in the child’s environment are engaged (e.g., teachers, probation officers).
Probably Efficacious (Level 2).
There are eleven probably efficacious categories, nine for Children and one for Adolescents with DB, and one for Adolescents with JJ-Involvement.
Two new treatment categories were added: Behavior Therapy delivered to families via the Internet (i.e., Internet-delivered PCIT), and Behavior Therapy and CBT focused on two-parent households that combine groups and individual sessions for both parents (i.e., Hitkashrut Parent Training Program). Additionally, a category previously labeled by Kaminski and Claussen (2017) as Parent Self-Directed Behavior Therapy was more clearly specified as Behavior Therapy that is parent self-directed combined with parent coaching (e.g., Strongest Families/Strongest Families SmartWebsite, 1–2–3 Magic, Incredible Years Self-Directed). Behavior Therapy delivered via multi-family groups (i.e., Group PCIT), individual parent sessions (i.e., unnamed behavioral training for foster parents), parent groups with child groups (i.e., Stop Now And Plan [SNAP]), and child sessions with parent participation (i.e., Problem-Solving Skills Training with in vivo practice [PSST-P]) remained probably efficacious (for a complete list of specific treatments see Supplemental Table 1 ). Also remaining were Behavior Therapy and Family Therapy combined and delivered via multi-family groups (i.e., Multiple Family Groups) and Emotion-Focused Therapy delivered via parent groups (i.e., Tuning Into Kids). Of note, one adjustment to Kaminski and Claussen’s leveling involved Behavior Therapy for children with DB conducted through parent groups and child groups. This category includes SNAP but was previously placed on Level 2 due to RCTs of other interventions; those interventions, however, required school-based components rather than being limited to family-based. The initial SNAP study alone did not meet the rigorous methods criteria to reach placement on Level 2. However, a more recent SNAP RCT does meet methods criteria, so the category remains on Level 2 for family-based treatments.
In brief, the Behavior Therapy and Behavior Therapy plus CBT treatments listed here continue to use the behavioral modification principles and cognitive problem-solving skills described for Level 1 treatments; however, the populations and delivery of the treatments are distinct. Emotion-Focused Therapy (EFT) for parents concentrates on parents learning more about their and their children’s emotions and how to have adaptive interactions and effective communication via emotion coaching. Common EFT techniques are empathetic listening; normalizing, mirroring, or reflecting; validation; redirection; and heightening of emotions.
Treatment incorporating Behavior Therapy, CBT, and Family Therapy delivered via a combination of family, parent, and child sessions (i.e., MST) remains probably efficacious . MST was described above.
Treatment incorporating Behavior Therapy, CBT, and Family Therapy delivered via family sessions (i.e., FFT) remains probably efficacious . FFT is delivered in clinic and home settings by trained and certified therapists assessing and intervening in youths’ risks and protective factors across their environments through five major components: engagement, motivation, relational assessment, behavior change, and generalization.
Possibly Efficacious (Level 3).
Based on the RCT criterion for Level 3, there are seven possibly efficacious treatment categories, two for Children and five for Adolescents with DB.
Treatments include Behavior Therapy via a combination of parent and child groups, family sessions, and individual child sessions (i.e., Project TEAM) and Behavior Therapy and CBT via parent groups (i.e., Rational Positive Parenting Program).
Two new treatment categories were added: Behavior Therapy via a parent self-directed approach (i.e., Parenting Toolkit) and Behavior Therapy, CBT, and Family Therapy delivered to families (i.e., FFT for DB). Three categories remain possibly efficacious : Behavior Therapy and Family Therapy via parent groups and family sessions (i.e., Familias Unidas), Behavior Therapy combined with CBT via family sessions (i.e., Support to Reunite, Involve, and Value Each Other [STRIVE]), and a combination of Behavior Therapy, CBT, and Family Therapy via individual parent sessions (i.e., Non-Violent Resistance). As noted in prior Levels, all of these use behavioral modification techniques and some combine CBT skills.
Currently, there are no possibly efficacious treatments.
In total, this review found 3 well-established , 11 probably efficacious , and 7 possibly efficacious treatment categories for family-based treatments of DB from childhood through adolescence (see Table 2 ). Expanding to include the full age range of childhood through adolescence and using the newest specification of evidence Levels to review all previous evidence up to April 2020, this review provides a significant update to the prior JMFT review on family-based treatments for DB ( Henggeler & Sheidow, 2012 ). This review included a broader range of RCTs (i.e., not limiting to adolescent treatments and to those with multiple, independent RCTs and sustained effects) and differentiated treatments for adolescents with JJ-involvement.
This update revealed some exciting advances. The large number of RCTs ( n = 27) for a single category of presenting problems is remarkable. Along with identifying a large number and type of RCT-tested family-based treatments, there was notable expansion in different methods of treatment settings (e.g., home), providers (e.g., caseworkers), countries (e.g., China, Portugal), and delivery (e.g., via Internet) represented. The field sometimes assumes that most RCTs take place in university settings and with higher-income participants that lack diversity, but nothing could be farther from the truth when seeing the RCT literature on DB. Indeed, many of the studies were conducted in community-based settings utilizing real-world providers and involving youth of considerable diversity in terms of biological sex, race, and ethnicity. For studies conducted in a JJ context, investigators ensure that judges and other JJ professionals do not require participation as that would be in direct violation of research ethics standards. Thus, these samples are likely very similar to the “real world” population of children and adolescents needing treatment. Finally, while many of the larger U.S.-based RCTs were likely costly and dependent upon large federal grants, that money appears well spent considering the focus on promoting individual and family health. Further and as described next, several RCTs took place outside the U.S., suggesting that high-quality treatment studies can be successfully completed without the financial backing of a large and well-resourced U.S. federal funding agency.
RCTs were conducted with families in a range of countries, suggesting replicability and cross-cultural generalizability for family-based treatments of DB. This is consistent with other work on cultural sensitivity and transportability of family interventions internationally (e.g., Kumpfer et al., 2012 ). It is encouraging that many of these RCTs were supportive. At the same time, two studies of well-established or probably efficacious treatments initially tested in the U.S. did not translate to significant differences beyond treatment as usual in the U.K. ( Fonagy et al., 2018 ; Humayun et al. 2017 ). This may reflect that usual care for U.K. teens involves substantial services compared to the U.S. Further, while international representation grew, most (albeit not all) of the countries represented have a history of conducting DB research. Future work should continue to test family-based treatments of DB in the larger international field.
Technology-facilitated interventions were more prevalent than in prior reviews. These can be less burdensome and more accessible ( Bishop et al., 2006 ), especially for families in low-resourced communities. Further, studies of consumer preference found parents to be interested in web-based alternatives to more traditional in-person services ( Metzler et al., 2012 ). That said, as shown in Table 1 , technology-based programs are not universally effective, highlighting the need for ongoing research on the essential elements of this innovative approach to treatment delivery.
A large majority (71%) of the recent trials focused on children rather than adolescents, and on treatments based in behavior therapy, which follows the trend in past research on DB. Many new RCTs lent further support to existing treatment categories, especially for Level 1 treatments for children, which already had substantive support (see Kaminski & Claussen, 2017 ). This highlights robust replicability for many of the family-based treatments making up these categories. Indeed, nearly all child-focused categories include multiple named treatments within the category, suggesting a healthy array of evidence-based treatment model options. Trials targeting children, versus adolescents, were also more likely to meet Supportive criteria, suggesting these family-based models are more easily replicated in childhood. Findings may reflect the more controlled and supervised environments of children (e.g., home, school) in comparison to adolescents, making change implemented mainly by caregivers easier to achieve.
In contrast, there is one well-established category for adolescents with JJ-involvement, no well-established treatments for adolescents with DB, and one probably efficacious category for adolescents, an increase from prior reviews. Notably, the evidence-based treatments at these upper two Levels for adolescent DB (i.e., MST, TFCO, FFT) can require significant support and resources for implementation, but also can lead to long-term societal cost savings. Expanding examination of treatments for adolescents who have DB without JJ-involvement is paramount given the near absence of options at Levels 1 and 2. One example from the current review that found support in the possibly efficacious Level is the Parenting Toolkit, a parent self-directed program delivered via the Internet for adolescents with DB, which was found to have superior outcomes compared to waitlist ( Irvine et al., 2015 ). With a convenient delivery and program style (i.e., non-sequential Internet instruction), it allows parents to work at their own pace and on topics relevant to them (e.g., stealing, grades, curfew). This and similar programs are in nascent stages of examination, so testing of both replicability and durability of outcomes is still needed.
Limitations
This review categorized treatments by type and delivery, consistent with prior reviews using Southam-Gerow and Prinstein (2014) Levels. While beneficial for identifying approaches that seem consistently better, interventions can vary widely in delivery and techniques. Most importantly, outcomes can vary for such treatments. Thus, caution is given against relying solely on the overall treatment categories. Additionally, no inter-rater reliability was tracked during article coding. This review also focused on summarizing the RCT literature which covers the criteria needed for the top Levels of Southam-Gerow and Prinstein. This RCT focus is warranted given it is a remarkably large literature, as well as since RCTs are the gold-standard in healthcare and DB has such a significant societal impact, but it is nonetheless a limitation. Indeed, there is a robust literature of non-RCT designs. The Southam-Gerow and Prinstein criteria also limits to samples that focus on clinically diagnosed DB, thus this review excluded studies designed to prevent DB and its many problems. Finally, while we aimed to be exhaustive and highly inclusive in our search and decision-making, our operationalization of the criteria may have excluded some studies. For instance, the authors of one Incredible Years RCT ( Karjalainen et al., 2019 ) identified a problem in statistical power, resulting in the study being excluded; although, this would not change results as the intervention already fully met the well-established category.
Practice Guidelines
Leaders of organizations looking to implement evidence-based treatments for DB have a menu of well-established and probably efficacious treatments from which to choose. However, there are crucial implementation factors to consider. Namely, treatment fidelity is essential to achieving desired outcomes (see McCart & Sheidow, 2016 ). If not delivered with fidelity, the expected outcomes may not be achieved, and there is little evidence of maintaining fidelity in the absence of a strong ongoing quality assurance system (e.g., Smith-Boydston et al., 2014 ). Given that, treatments identified are transported through purveyor organizations that attempt to ensure high-quality training and support to maintain fidelity. Communities, healthcare organizations, and agencies can seek information for implementing these models from those purveyors.
Additionally, a number of treatments identified also have proven cost-effectiveness (although this is beyond the scope of the current review), further informing decision-making by such community members and leadership. Aside from implementing one of the treatments in full, the descriptions published by treatment developers can be used to delineate some strategies for clinical work, with the caveat that clinicians and organizations are not free to conclude they are delivering the named treatment without validated verification of such. Also, when embarking on implementing a new treatment, even if it has been designated as well-established or probably efficacious , it will be important to consider carefully the research support and characteristics of the samples, locations, and providers for which it has been rigorously tested to determine if it could be a good fit for the proposed setting. That is, even though there is expansion, much of the supportive overall evidence base comes from selected populations (e.g., American children, JJ-involved adolescents) and providers (e.g., PhD and Master’s professionals).
Conclusions and Future Directions
This review builds on the past literature and identified a number of evidence-based treatment categories. The findings suggest several considerations for future research on family-based treatments. Few new treatments were tested in recent RCTs, but rather the research focused on replications. While this approach has advantages as these programs continue to build a larger evidence base, the development and testing of treatments for specific population gaps (e.g., adolescents without JJ-involvement) or cultural modifications of current treatments to ensure success in a broader array of populations is an important next step.
Future studies should consider treatment durability (i.e., maintenance of treatment gains); the bulk of RCTs continue to assess outcomes at posttreatment only or were limited to short-term follow-up ( range = 1–36 months; median = 6 months). Length of treatment also is interesting. While there are exceptions, the RCTs of brief family-based treatments suggested such treatments may not be powerful enough to generate DB improvement. DB is a complex phenomenon often affecting multiple settings (e.g., school, home, peer relationships). In contrast to findings on other psychiatric problems or broader prevention samples (e.g., Schleider & Weisz, 2017 ; Tully & Hunt, 2016 ), DB treatments may need multiple sessions to target the nuances in these settings, and to give caregivers time to practice and receive feedback on their efforts in between sessions.
Reliance on waitlist or no-treatment comparison (versus active comparison) in several RCTs was a limiting factor for establishing well-established and probably efficacious treatments, as was the lack of rigorous methods like intent-to-treat research (e.g., assessing only treatment completers). Beyond factors determining evidence base Levels, studies also tended to be limited to parent-report measures, which may be biased when the parent is the one receiving the intervention. Finally, there is a continued need for determining mechanisms of action for DB treatments, potentially within the context of rigorous RCTs and/or via advanced experimental methods such as manipulation-of-mediator designs (e.g., Pirlott & MacKinnon, 2016 ).
While there are still clear areas in need of expansion and closer consideration, family-based treatments for DB, particularly for children and for adolescents with JJ-involvement, have robust evidence from gold-standard rigorous research. Moreover, the evidence suggesting that these treatments can be delivered to varying locations, cultures, and populations is encouraging.
Supplementary Material
Acknowledgements:.
The authors would like to thank Colleen Walsh, Jenene Peterson, and Jessica Hughitt for assisting with the literature review.
The authors’ effort in the preparation of this publication was supported by grants from the National Institutes of Health under award numbers R01DA041434 (Ashli J. Sheidow), R01DA043578 (Mike R. McCart), and K23DA048161 (Tess K. Drazdowski). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest: The authors declare they have no conflict of interest.
Note: References from Table 1 (i.e., studies identified since prior review [2014-April 2020]) are marked with an asterisk.
- *. Baker S, Sanders MR, Turner KMT, & Morawska A (2017). A randomized controlled trial evaluating a low-intensity interactive online parenting intervention, Triple P Online Brief, with parents of children with early onset conduct problems. Behaviour Research and Therapy, 91, 78–90. [ DOI ] [ PubMed ] [ Google Scholar ]
- Baldwin SA, Christian S, Berkeljon A, & Shadish WR (2012). The effects of family therapies for adolescent delinquency and substance abuse: A meta‐analysis. Journal of Marital and Family Therapy, 38(1), 281–304. [ DOI ] [ PubMed ] [ Google Scholar ]
- Bishop D, Bryant KS, Giles SM, Hansen WB, & Dusenbury L (2006). Simplifying the delivery of a prevention program with web-based enhancements. The Journal of Primary Prevention, 27(4), 433–444. [ DOI ] [ PubMed ] [ Google Scholar ]
- *. Bjørseth Å, & Wichstrøm L (2016). Effectiveness of Parent-Child Interaction Therapy (PCIT) in the treatment of young children’s behavior problems. A randomized controlled study. PloS One, 11(9), E0159845. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- *. Burke J, & Loeber R (2015). The Effectiveness of the Stop Now and Plan (SNAP) program for boys at risk for violence and delinquency. Prevention Science, 16(2), 242–253. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Colman I, Murray J, Abbott RA, Maughan B, Kuh D, Croudace TJ, & Jones PB (2009). Outcomes of conduct problems in adolescence: 40 year follow-up of national cohort. BMJ (Clinical research ed.), 338, a2981. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- *. Comer JS, Furr JM, Miguel EM, Cooper-Vince CE, Carpenter AL, Elkins RM, Kerns CE, Cornacchio D, Chou T, Coxe S, DeSerisy M, Sanchez AL, Golik A, Martin J, Myers KM, & Chase R (2017). Remotely delivering real-time parent training to the home: An initial randomized trial of Internet-delivered parent-child interaction therapy. Journal of Consulting and Clinical Psychology, 85(9), 909–917. [ DOI ] [ PubMed ] [ Google Scholar ]
- *. Dadds MR, Thai C, Mendoza Diaz A, Broderick J, Moul C, Tully LA, Hawes DJ, Davies S, Burchfield K, & Cane L (2019). Therapist-assisted online treatment for child conduct problems in rural and urban families: Two randomized controlled trials. Journal of Consulting and Clinical Psychology, 87(8), 706–719. [ DOI ] [ PubMed ] [ Google Scholar ]
- Erskine HE, Ferrari AJ, Polanczyk GV, Moffitt TE, Murray CJ, Vos T, Whiteford HA, & Scott JG (2014). The global burden of conduct disorder and attention‐deficit/hyperactivity disorder in 2010. Journal of Child Psychology and Psychiatry, 55(4), 328–336. [ DOI ] [ PubMed ] [ Google Scholar ]
- *. Elizur Y, Somech LY, & Vinokur AD (2017). Effects of parent training on callous-unemotional traits, effortful control, and conduct problems: Mediation by parenting. Journal of Abnormal Child Psychology, 45(1), 15–26. [ DOI ] [ PubMed ] [ Google Scholar ]
- Eyberg SM, Nelson MM, & Boggs SR (2008). Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child & Adolescent Psychology, 37(1), 215–237. [ DOI ] [ PubMed ] [ Google Scholar ]
- Fleming CB, Catalano RF, Haggerty KP, & Abbott RD (2010). Relationships between level and change in family, school, and peer factors during two periods of adolescence and problem behavior at age 19. Journal of Youth and Adolescence, 39(6), 670–682. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- *. Fonagy P, Butler S, Cottrell D, Scott S, Pilling S, Eisler I, Fuggle P, Kraam A, Byford S, Wason J, Ellison R, Simes E, Ganguli P, Allison E, & Goodyer IM (2018). Multisystemic therapy versus management as usual in the treatment of adolescent antisocial behaviour (START): A pragmatic, randomised controlled, superiority trial. The Lancet Psychiatry, 5(2), 119–133. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- *. Ghaderi A, Kadesjö C, Björnsdotter A, & Enebrink P (2018). Randomized effectiveness trial of the Family Check-Up versus Internet-delivered Parent Training (iComet) for families of children with conduct problems. Scientific Reports, 8(1), 11486. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ghandour RM, Sherman LJ, Vladutiu CJ, Ali MM, Lynch SE, Bitsko RH, & Blumberg SJ (2019). Prevalence and treatment of depression, anxiety, and conduct problems in US children. The Journal of Pediatrics, 206, 256–267. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- *. Hartnett D, Carr A, & Sexton T (2016). The effectiveness of Functional Family Therapy in reducing adolescent mental health risk and family adjustment difficulties in an Irish context. Family Process, 55(2), 287–304. [ DOI ] [ PubMed ] [ Google Scholar ]
- *. Helander M, Lochman J, Högström J, Ljótsson B, Hellner C, & Enebrink P (2018). The effect of adding Coping Power Program-Sweden to Parent Management Training-effects and moderators in a randomized controlled trial. Behaviour Research and Therapy, 103, 43–52. [ DOI ] [ PubMed ] [ Google Scholar ]
- Henggeler SW, & Sheidow AJ (2012). Empirically supported family-based treatments for conduct disorder and delinquency in adolescents. Journal of Marital and Family Therapy, 38(1), 30–58. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- *. Hogue A, Dauber S, Henderson CE, Bobek M, Johnson C, Lichvar E, & Morgenstern J (2015). Randomized trial of Family Therapy vs Nonfamily Treatment for adolescent behavior problems in usual care. Journal of Clinical Child & Adolescent Psychology, 44, 954–969. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hockenberry S, & Puzzanchera C (2018). Juvenile court statistics 2016. Pittsburgh, PA: National Center for Juvenile Justice. [ Google Scholar ]
- *. Homem TC, Gaspar MF, Santos MJS, Azevedo AF, & Canavarro MC (2015). Incredible Years Parent Training: Does it improve positive relationships in Portuguese families of preschoolers with oppositional/defiant symptoms? Journal of Child and Family Studies, 24(7), 1861–1875. [ Google Scholar ]
- *. Humayun S, Herlitz L, Chesnokov M, Doolan M, Landau S, & Scott S (2017). Randomized controlled trial of Functional Family Therapy for offending and antisocial behavior in UK youth. Journal of Child Psychology and Psychiatry, 58(9), 1023–1032. [ DOI ] [ PubMed ] [ Google Scholar ]
- *. Irvine AB, Gelatt VA, Hammond M, & Seeley JR (2015). A randomized study of internet parent training accessed from community technology centers. Prevention Science, 16(4), 597–608. [ DOI ] [ PubMed ] [ Google Scholar ]
- *. Jonkman CS, Schuengel C, Oosterman M, Lindeboom R, Boer F, & Lindauer RJL (2017). Effects of Multidimensional Treatment Foster Care for Preschoolers (MTFC-P) for young foster children with severe behavioral disturbances. Journal of Child and Family Studies, 26(5), 1491–1503. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kaminski JW, & Claussen AH (2017). Evidence base update for psychosocial treatments for disruptive behaviors in children. Journal of Clinical Child & Adolescent Psychology, 46(4), 477–499. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Karjalainen P, Kiviruusu O, Aronen ET, & Santalahti P (2019). Group-based parenting program to improve parenting and children’s behavioral problems in families using special services: A randomized controlled trial in a real-life setting. Children and Youth Services Review, 96, 420–429. [ Google Scholar ]
- Kaslow NJ, Broth MR, Smith CO, & Collins MH (2012). Family‐based interventions for child and adolescent disorders. Journal of Marital and Family Therapy, 38(1), 82–100. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kumpfer KL, Magalhães C, & Xie J (2012). Cultural adaptations of evidence-based family interventions to strengthen families and improve children’s developmental outcomes European Journal of Developmental Psychology, 9, 104–116. [ Google Scholar ]
- Lahey BB, Schwab-Stone M, Goodman SH, Waldman ID, Canino G, Rathouz PJ, Miller TL, Dennis KD, Bird H, & Jensen PS (2000). Age and gender differences in oppositional behavior and conduct problems: A cross-sectional household study of middle childhood and adolescence. Journal of Abnormal Psychology, 109(3), 488. [ PubMed ] [ Google Scholar ]
- *. Leung C, Tsang S, Sin TCS, & Choi S (2015). The efficacy of Parent–Child Interaction Therapy with Chinese families: Randomized controlled trial. Research on Social Work Practice, 25(1), 117–128. [ Google Scholar ]
- *. Lochman JE, Baden RE, Boxmeyer CL, Powell NP, Qu L, Salekin KL, & Windle M (2014). Does a booster intervention augment the preventive effects of an abbreviated version of the Coping Power Program for aggressive children? Journal of Abnormal Child Psychology, 42(3), 367–381. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- *. Maaskant AM, van Rooij FB, Overbeek GJ, Oort FJ, & Hermanns JMA (2016). Parent training in foster families with children with behavior problems: Follow-up results from a randomized controlled trial. Children and Youth Services Review, 70, 84–94. [ Google Scholar ]
- McCart MR, & Sheidow AJ (2016). Evidence-based psychosocial treatments for adolescents with disruptive behavior. Journal of Clinical Child & Adolescent Psychology, 45(5), 529–563. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Metzler CW, Sanders MR, Rusby JC, & Crowley RN (2012). Using consumer preference information to increase reach and impact of media-based parenting interventions in a public health approach to parenting support. Behavior Therapy, 43(2), 257–270. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- *. Morpeth L, Blower S, Tobin K, Taylor RS, Bywater T, Edwards RT, Axford N, Lehtonen M, Jones C, & Berry V (2017). The effectiveness of the Incredible Years pre-school parenting programme in the United Kingdom: A pragmatic randomised controlled trial. Child Care in Practice, 23(2), 141–161. [ Google Scholar ]
- *. Multisite Violence Prevention Project. (2014). Targeting high-risk, socially influential middle school students to reduce aggression: Universal versus selective preventive intervention effects. Journal of Research on Adolescence, 24(2), 364–382. [ Google Scholar ]
- *. Olthuis JV, McGrath PJ, Cunningham CE, Boyle MH, Lingley-Pottie P, Reid GJ, Bagnell A, Lipman EL, Turner K, Corkum P, Stewart SH, Berrigan P, & Sdao-Jarvie K (2018). Distance-delivered parent training for childhood disruptive behavior (Strongest Families): A randomized controlled trial and economic analysis. Journal of Abnormal Child Psychology, 46(8), 1613–1629. [ DOI ] [ PubMed ] [ Google Scholar ]
- *. Palmer ML, Keown LJ, Sanders MR, & Henderson M (2019). Enhancing outcomes of low-intensity parenting groups through sufficient exemplar training: A randomized control trial. Child Psychiatry & Human Development, 50(3), 384–399. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pirlott AG & MacKinnon DP (2016). Design approaches to experimental mediation. Journal of Experimental Social Psychology, 66, 29–38. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- *. Porzig-Drummond R, Stevenson RJ, & Stevenson C (2014). The 1–2–3 Magic parenting program and its effect on child problem behaviors and dysfunctional parenting: A randomized controlled trial. Behaviour Research and Therapy, 58, 52–64. [ DOI ] [ PubMed ] [ Google Scholar ]
- Schleider JL, & Weisz JR (2017). Little treatments, promising effects? Meta-analysis of single-session interventions for youth psychiatric problems. Journal of the American Academy of Child & Adolescent Psychiatry, 56(2), 107–115. [ DOI ] [ PubMed ] [ Google Scholar ]
- Smith-Boydston JM, Holtzman RJ, & Roberts MC (2014). Transportability of multisystemic therapy to community settings: Can a program sustain outcomes without MST services oversight? Child Youth Care Forum, 43(5), 593–605. [ Google Scholar ]
- *. Sourander A, McGrath PJ, Ristkari T, Cunningham C, Huttunen J, Lingley-Pottie P, Hinkka-Yli-Salomäki S, Kinnunen M, Vuorio J, Sinokki A, Fossum S, & Unruh A (2016). Internet-Assisted Parent Training Intervention for disruptive behavior in 4-year-old children: A randomized clinical trial. JAMA Psychiatry, 73(4), 378–387. [ DOI ] [ PubMed ] [ Google Scholar ]
- *. Sourander A, McGrath PJ, Ristkari T, Cunningham C, Huttunen J, Hinkka-Yli-Salomäki S, Kurki M, & Lingley-Pottie P (2018). Two-year follow-up of Internet and Telephone Assisted Parent Training for disruptive behavior at age 4. Journal of the American Academy of Child & Adolescent Psychiatry, 57(9), 658–668.e1. [ DOI ] [ PubMed ] [ Google Scholar ]
- Southam-Gerow MA, & Prinstein MJ (2014). Evidence base updates: The evolution of the evaluation of psychological treatments for children and adolescents. Journal of Clinical Child & Adolescent Psychology, 43(1), 1–6. [ DOI ] [ PubMed ] [ Google Scholar ]
- Tully LA, & Hunt C (2016). Brief parenting interventions for children at risk of externalizing behavior problems: A systematic review. Journal of Child and Family Studies, 25, 705–719. [ Google Scholar ]
- *. Van Holen F, Vanschoonlandt F, & Vanderfaeillie J (2017). Evaluation of a foster parent intervention for foster children with externalizing problem behaviour: Evaluation of a foster parent intervention. Child & Family Social Work, 22(3), 1216–1226. [ Google Scholar ]
- *. Webb HJ, Thomas R, McGregor L, Avdagic E, & Zimmer-Gembeck MJ (2017). An evaluation of parent-child interaction therapy with and without motivational enhancement to reduce attrition. Journal of Clinical Child & Adolescent Psychology, 46(4), 537–550. [ DOI ] [ PubMed ] [ Google Scholar ]
- *. Weeland J, Chhangur RR, van der Giessen D, Matthys W, de Castro BO, & Overbeek G (2017). Intervention effectiveness of The Incredible Years: New insights into sociodemographic and intervention-based moderators. Behavior Therapy, 48(1), 1–18. [ DOI ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- View on publisher site
- PDF (641.8 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Behavior modification.
Hannah K. Scott ; Ankit Jain ; Mark Cogburn .
Affiliations
Last Update: July 10, 2023 .
- Continuing Education Activity
Behavior modification is a psychotherapeutic intervention primarily used to eliminate or reduce maladaptive behavior in children or adults. While some therapies focus on changing thought processes that can affect behavior, behavior modification focuses on changing specific behaviors with little consideration of a person’s thoughts or feelings. The progress and outcome of the intervention can be measured and evaluated. First, a functional analysis of the antecedents and consequences of the problem behavior(s) must be identified. This allows for the determination of specific target behaviors that will become the focus of treatment. Then, certain variables can be manipulated via reinforcers and punishments to change problem behavior(s). The goal is to eliminate or reduce maladaptive behavior. This activity reviews the indications and contraindications for behavior modification and highlights the role of the interprofessional team in the management of patients with behavioral disorders.
- Identify the indications for behavioral modification therapy.
- Describe the contraindications to behavior modification therapy.
- Outline the clinical utility of behavioral modification therapy.
- Explain interprofessional team strategies for improving care coordination and communication to advance the use of behavioral modification therapy and improve patient outcomes.
- Introduction
Behavior modification is a psychotherapeutic intervention primarily used to eliminate or reduce maladaptive behavior in children or adults. While some therapies focus on changing thought processes that can affect behavior, for example, cognitive behavioral therapy, behavior modification focuses on changing specific behaviors with little consideration of a person’s thoughts or feelings. The progress and outcome of the intervention can be measured and evaluated. Functional analysis of the antecedents and consequences of the problem behavior(s) must be identified. This leads to the creation of specific target behaviors that will become the focus of change. Then, certain variables can be manipulated via reinforcers and punishments to change problem behavior(s). The goal is to eliminate or reduce maladaptive behavior. [1] [2] [3]
Behavior modification is a type of behavior therapy. B. F. Skinner demonstrated that behavior could be shaped through reinforcement and/or punishment. Skinner noted that a reinforcer is a consequence that increases the likelihood of behavior to recur, while punishment is a consequence that decreases the chance. Positive and negative are used in mathematical terms. Positive indicates that something is added, and negative indicates something is subtracted or taken away. Thus, positive reinforcement occurs when a behavior is encouraged by rewards. If a child enjoys candy and cleaning the room is the desired behavior, the candy is a positive reinforcer (reward) because it is something that is given or added when the behavior occurs. This makes the behavior more likely to recur. Negative reinforcement is removing a stimulus as the consequence of behavior but results in a positive outcome for the individual. For example, a fine is dropped, and a person no longer has to go to jail. The removal of the negative stimulus (the fine) results in a positive outcome for the individual, no jail time.
Conversely, positive punishment is the addition of an adverse consequence. For example, a child gets spanked when he crosses the street without holding his mother’s hand. He then no longer crosses the street alone. Spanking is positive punishment because it is a consequence added to the situation that decreases the likelihood of the child crossing the street alone. Negative punishment is taking away favorable consequences to reduce unwanted behavior. For example, if Emily doesn’t finish her homework on time, her cell phone gets taken away. She makes it a priority to finish her homework immediately after school before she does anything else. Removal of the cell phone would be a “negative” because it takes something away, decreasing the chance that she won’t finish her homework the next time.
Reinforcement and punishment both work independently, as well as together, as part of a behavior plan. Positive reinforcement works exceedingly better and faster than punishment. In child psychiatry, parents often come to the office angry and frustrated with their child because “nothing works.” They have tried multiple types of punishments when bad behavior has occurred using the removal of toys or privileges away or placing a child in time out. Often positive types are not being reinforced. One immediate benefit of behavior modification plans is the shift away from solely punishing unwanted behavior to also rewarding good behavior.
(Table 1, Scott and Cogburn, 2017)
In table 1, note that punishment and reinforcement have nothing to do with good or bad behavior, only if it increases or decreases the likelihood of the behavior to recur.
There are several schedules of reinforcement that can impact behavior. When a behavior plan is initially set up, continuous two is used to establish and reinforce the behavior. Once the behavior has been established, continuous reinforcement can change to intermittent reinforcement which is termed thinning . There are four types of intermittent reinforcement. They are:
- Fixed interval where the person is reinforced by a set number of responses
- Variable interval where the person is reinforced by a variable number of responses
- Fixed ratio where the person is reinforced after a certain number of responses
- Variable ratio where the person is reinforced after a variable number of responses. Variable ratio intermittent reinforcement is the most effective schedule to reinforce a behavior.
Examples
- Fixed interval: rewarding a person at the end of each day
- Variable interval: rewarding a person sometimes at the end of the day, sometimes at the end of the week, sometimes every few days
- Fixed ratio: rewarding a person after completing the desired behavior four times
- Variable ratio: rewarding a person after completing the desired behavior after three times, then after six times, then after two times. Gambling is a real-world example of a variable ratio of reinforcement.
- Indications
The indications for developing a behavior modification plan can be for any unwanted, maladaptive, or aberrant behavior. It can also be used to teach and reinforce new, desired behaviors. In clinical settings, the treatment team utilizes the concept of operant conditioning to reinforce prosocial behaviors through positive consequences as seen in token economy, shaping, differential reinforcement of desired behaviors, and extinguish the undesired behaviors through negative consequences like an overcorrection, response costs, time outs.
In child psychiatry, behavior modification is often part of treatment planning when a child is diagnosed with attention-deficit hyperactivity disorder (ADHD), oppositional defiant disorder, conduct disorder, intermittent explosive disorder, or other externalizing disorders (as opposed to internalizing disorders like major depression). While behavior therapy is not limited to externalizing behavior disorders, it is often a key part of the treatment plan because the presenting problem is behavior-related. [4] [5] [6] [7] .
Applied Behavioral Analysis (ABA) is one of the common therapeutic techniques used in behavior modification. It has been proven very effective in those diagnosed with autism spectrum disorders and other similar developmental disorders.
Behavior modification is also a component of Parent-Child Interaction Therapy (PCIT), which teaches specific skills to the parents that they can use to help improve physical and verbal exchanges with their children. PCIT is an evidence-based intervention for preventing child abuse & neglect, helpful for children who exhibit disruptive behavior and/or have experienced trauma, those on the autism spectrum, and has been shown to decrease child’s risk of antisocial and criminal behavior later in life.
The Triple P – Positive Parenting Program draws on social learning, cognitive therapy, behavioral modification, and developmental theory as well as an exploration into risk factors associated with the development of social and behavioral problems in children. It aims to empower parents with the skills and confidence they need to be self-sufficient and to be able to manage family issues without ongoing support.
Many reviews and metaanalyses of the research literature have established that behavioral treatments—including brief intervention, marital and family therapy, behavioral couples therapy, relapse prevention, and other cognitive-behavioral treatments in addition to community reinforcement and contingency management approaches—are among the most effective treatments for AUDs [8] [9]
- Contraindications
A behavior plan should not be started if it cannot be appropriately executed with consistency and longevity. Often, shaping, which is reinforcing and rewarding behavior as it approaches the desired behavior, is needed before the desired behavior is fully reached. Perfection cannot be the expectation from a behavior plan. Mistakes and setbacks are common when a change in behavior is expected, so consistency and patience are important from the caretakers and the clinician. If a behavior plan is only partially enforced, then this can lead to worsening behavior.
A behavior modification chart is frequently used when implementing a behavior modification plan. Behavior charts require specific, objective, quantifiable tasks that are rewarded in a previously agreed upon way, be it points, stickers, or tally marks.
(Table 2, Scott and Cogburn, 2017)
- 3 points per day equal 30 min of screen time
- 6 points per day equal 1 hour of screen time
- 20 points per week equal picking a toy worth $5 to $10 at the store
- 25 points per week equal the toy plus getting to stay up 2 hours later on Saturday night.
(The above behavior chart with the subsequent rewards would be appropriate for a five to ten-year-old)
A “token economy” is synonymous with a behavior modification plan. A token (sticker, chip, point, tally) is anything that can be earned by exhibiting the desired behavior that can then be exchanged for reinforcers.
Reinforcers or rewards are a key part of a behavior plan but are unique to each child. The reinforcement has to be of value to the child for the program to be effective. A child may be motivated to make her bed every day if she gets a sucker every time she does it, but she may not make her bed if she gets extra reading time. She has to value the reward for the reward to be valued.
Reinforcers and punishments must happen at the time of the behavior to increase the likelihood of success of a behavior modification plan. The more immediate to the behavior the better. For example, praising a child for using the toilet while he is using it versus later that day. The reinforcer must be appropriate, e.g., giving a child a sticker every time he says please, or giving a teenager extra screen time for a good attitude. And lastly, the reinforcer must be consistent where the behavior is rewarded by all caretakers as previously agreed upon and not to avoid punishment due to caretaker guilt or inconvenience.
A behavior modification plan can be started and implemented with an individual or by a team of people. A parent, teacher, or childcare provider can start a plan. Often, the behavior plan can be implemented in multiple settings, like at school and home (rewards for turning in homework assignments to the teacher, and rewards for cleaning your room by the parent). The broader the settings for the behavior plan, the better.
- Preparation
Time is needed to define the problem behavior. Then the desired behavior has to be decided upon with appropriate rewards. If punishment is considered, specific punishments should go along with specific aberrant behavior.
- Technique or Treatment
The mainstay of behavior modification plans is consistency.
- Complications
Resistance in the beginning, from both the child and the parent or teacher, is to be expected. Children are often opposed to trying anything new because they are tired of being punished and reprimanded for their aberrant behavior. They do not want any more privileges or items taken away or banished. They may have low self-esteem or lack confidence that they can adequately fulfill the behavior plan. This is where shaping is important. If they come close to achieving the desired behavior, they can be rewarded in part or whole for their effort with the goal to one day reach the goal fully.
Parents or authority figures are sometimes resistant because they are angry or frustrated with the child and do not want to reward them for positive behavior. They may also be worried that it will not work. It may be a new way of thinking which is challenging and requires work to enforce consistently.
- Clinical Significance
Behavior therapy achieves goals in therapy that medication alone may not be able to accomplish. It has long-lasting effects on the individual even after the behavior plan is no longer in place because the new behavior is already established. Behavior can change the way a person thinks and feels about themselves which in psychiatry is an ultimate goal. [10] [11] [12] [13] [11]
- Enhancing Healthcare Team Outcomes
A behavior modification plan can be started and implemented with an individual or by a team of individuals that includes the mental health nurse, psychologist, social workers, primary care provider, parent, teacher, or childcare provider. Often, the behavior plan can be implemented in multiple settings, like at school and home (rewards for turning in homework assignments to the teacher, and rewards for cleaning your room by the parent). The broader the settings for the behavior plan, the better. Interprofessional involvement has been shown to improve health care quality and outcomes for patients, clients, families, and caregivers.
Behavior therapy achieves goals in therapy that medication alone may not be able to accomplish. It has long-lasting effects on the individual even after the behavior plan is no longer in place because the new behavior is already established. Behavior can change the way a person thinks and feels about themselves which in psychiatry is an ultimate goal.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Behavior Modification Chart Contributed by Hannah Scott
Behavior modification techniques Contributed by Ankit Jain, MD
Disclosure: Hannah Scott declares no relevant financial relationships with ineligible companies.
Disclosure: Ankit Jain declares no relevant financial relationships with ineligible companies.
Disclosure: Mark Cogburn declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Scott HK, Jain A, Cogburn M. Behavior Modification. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. [Cochrane Database Syst Rev. 2022] Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, et al. Cochrane Database Syst Rev. 2022 Feb 1; 2(2022). Epub 2022 Feb 1.
- Peer Play. [StatPearls. 2024] Peer Play. Scott HK, Cogburn M. StatPearls. 2024 Jan
- Does a negative discriminative stimulus function as a punishing consequence? [J Exp Anal Behav. 2018] Does a negative discriminative stimulus function as a punishing consequence? Bland VJ, Cowie S, Elliffe D, Podlesnik CA. J Exp Anal Behav. 2018 Jul; 110(1):87-104. Epub 2018 Jun 21.
- Review Evidence Brief: Comparative Effectiveness of Appointment Recall Reminder Procedures for Follow-up Appointments [ 2015] Review Evidence Brief: Comparative Effectiveness of Appointment Recall Reminder Procedures for Follow-up Appointments Peterson K, McCleery E, Anderson J, Waldrip K, Helfand M. 2015 Jul
- Review Comparative learning theory and its application in the training of horses. [Equine Vet J Suppl. 1998] Review Comparative learning theory and its application in the training of horses. Cooper JJ. Equine Vet J Suppl. 1998 Nov; (27):39-43.
Recent Activity
- Behavior Modification - StatPearls Behavior Modification - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Selectively reviewed problem-solving theory and research for possible applications in behavior modification. Problem solving was defined as a behavioral process which (a) makes available a variety of response alternatives for dealing with a problematic situation, and (b) increases the probability of selecting the most effective response from ...
Problem Solving* Programmed Instructions as Topic Psychological Theory Psychology, Clinical Research Set, Psychology
The BCTs that were most frequently linked to an MoA were “Instruction on How to Perform the Behavior” (182 times) and “Problem Solving” (177 times). The most frequently linked MoA was “Beliefs about Capabilities” (734 times), followed by “Intention” (318 times).
This article reviews the empirical literature to date on family-based treatments for children and adolescents with disruptive behavior (DB) problems. Such behavior is prevalent and costly, and it is a common reason for referrals to mental health treatment and/or the juvenile justice (JJ) system.
Behavior modification is a psychotherapeutic intervention primarily used to eliminate or reduce maladaptive behavior in children or adults. While some therapies focus on changing thought processes that can affect behavior, behavior modification focuses on changing specific behaviors with little consideration of a person’s thoughts or feelings.
This article reviews the theoretical models guiding research, the development of normative and atypical social problem solving, and the connection between social information processing and individual differences in functioning and concludes with a summary of efficacy of programs aimed at preventing social informationprocessing biases or ...